Psycho-Oncology and Palliative Care
Session: Poster Session
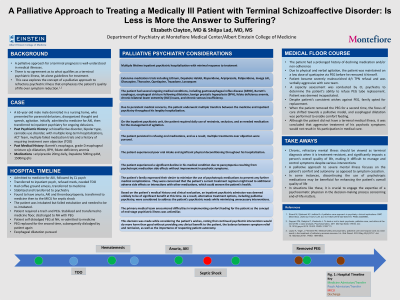
(121) Palliative Approach to Treating a Medically Ill Patient with Terminal Schizoaffective Disorder: Is Less is More the Answer to Suffering?
Trainee Involvement: Yes

Elizabeth Clayton, MD (she/her/hers)
Resident
Montefiore Medical Center
New York, New York, United States
Shilpa Lad, MD, MS
Attending Psychiatrist, Assistant Professor of Psychiatry
Albert Einstein College of Medicine, Montefiore Medical Center
New York, New York, United States
Presenting Author(s)
Co-Author(s)
Introduction Should we view the suffering associated with refractory mental illness as on par with end-of-life suffering? This case emphasizes the concept of end stage psychiatric illness, well-understood in medical conditions, and highlights the potential harm of psychiatric treatment in patients with refractory psychiatric illness. We explore the palliative approach to psychiatry that prioritizes the patient's quality of life and utilizes harm reduction strategies over symptom remission (Strand, 2020). Case The patient is a 65 y.o black male with medical history of Barrett's esophagus, esophageal stricture s/p dilatation, anemia, psychiatric history of schizoaffective disorder, multiple long-term psychiatric hospitalizations, and failed medication trials, admitted to the psychiatric unit for paranoid delusions. Patient's hospital course was complicated by multiple medical events, and his behavior became increasingly agitated when he refused medications. Despite obtaining a court order for treatment over objection, the patient's psychiatric symptoms showed minimal improvement, while his dysphagia, anemia and thrombocytopenia deteriorated due to side effects of psychotropic medications. Patient was transferred to ICU for septic shock, required intubation and PEG tube insertion. When he was considered suitable for the general medical floor, psychiatry was consulted for verbal and physical agitation. After failing six antipsychotics with no improvement, the family agreed to switch from a curative to a palliative approach. Therefore, our goal for this patient was to alleviate symptoms and reduce distress. (Lopez, 2010). Following the patient's removal of the PEG tube and display of verbal aggression, a capacity assessment was requested. Despite the patient's consistent wishes against PEG placement, the family initially felt that the replacement should be pursued. This would enable the administration of anxiolytics to keep the patient calm and potentially improve his nutritional status. However, after the patient dislodged the PEG tube for the second time, esophageal dilatation was pursued instead. The patient's desire for comfort feeds was deemed more important than PEG over objection. This was challenging for the primary team as the patient was not terminally ill and the team still held onto the belief that further psychiatric stabilization would ultimately improve his medical status. The concept of end stage psychiatric illness was unfamiliar. This case demonstrates the use of a palliative approach in managing a chronic, refractory psychosis. It highlights the valuable contribution of a psychosomatic physician in end-of-life decision-making, particularly in recognizing that a psychiatric illness can be considered terminal. The primary focus of the care team was on ensuring the patient's safety and comfort, rather than solely pursuing symptom relief. The decision to discontinue psychotropic medications and respect the patient's wish to preserve autonomy was made in order to enhance his quality of life. Strand M, Sjöstrand M, Lindblad A. A palliative care approach in psychiatry: clinical implications. BMC Med Ethics. 2020 Apr 19;21(1):29. doi:10.1186/s12910-020-00472-8. PMID:32306966. Lopez A, Yager J, Feinstein RE. Medical futility and psychiatry: palliative care and hospice care as a last resort in the treatment of refractory anorexia nervosa. Int J Eat Disord. 2010 May;43(4):372-7. doi:10.1002/eat.20701. PMID:19444903.
References:

