Psychopharmacology and Toxicology
Session: Poster Session
(152) Pathophysiology and Management of Risperidone-induced Sialorrhea
Trainee Involvement: Yes

Tyler J. Torrico, MD (he/him/his)
Clinical Fellow
National Institute of Mental Health
San Francisco, California, United States
Presenting Author(s)
Background
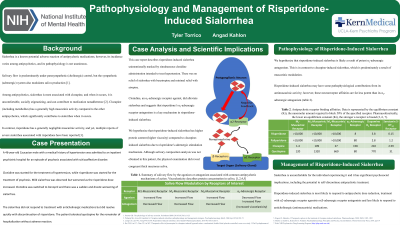
Among antipsychotics, sialorrhea is most associated with clozapine, and when it occurs, it is uncomfortable, socially stigmatizing, and can contribute to medication nonadherence. Risperidone has a generally negligible muscarinic activity compared to clozapine, and yet, multiple reports of severe sialorrhea associated with risperidone have been reported.
Case Presentation
This case report describes risperidone-induced sialorrhea that was unintentionally masked by simultaneous clonidine administration that was intended to treat hypertension. Interestingly, sialorrhea was present but mild when clonidine was present; however, when risperidone was further titrated and clonidine removed, a significant worsening of sialorrhea developed. Sialorrhea did not respond to treatment with anticholinergic medication.
Conclusion
The pathophysiology of antipsychotic-induced sialorrhea is complex and varies between antipsychotics. Risperidone-induced sialorrhea has prominent adrenergic pathophysiology that is composed of highly viscoelastic saliva (high protein content), differing from the more commonly encountered clozapine-induced sialorrhea. Risperidone-induced sialorrhea is more likely to respond to dose reduction, treatment with α2-adrenergic receptor agonists, and β-adrenergic receptor antagonists and less likely to respond to anticholinergic (antimuscarinic) medications.

