Neurocognitive Disorders, Delirium, and Neuropsychiatry
Session: Poster Session
(104) Postpartum Delirium and Near-Death Experience: A Case of Surviving a Complicated Delivery
Trainee Involvement: Yes
.jpg)
Sean E. Oldak, MD
Resident Physician
University of Miami Miller School of Medicine
Miami, Florida, United States
Omar Munoz Abraham, MD
PGY-4 Resident
University of Miami
Miami, Florida, United States.jpg)
Vanessa Padilla, MD
CL Psychiatry Fellowship Program Director
University of Miami
Miami, Florida, United States
Lujain Alhajji, MD
Assistant Professor
University of Miami
Miami, Florida, United States
Presenting Author(s)
Co-Author(s)
Background
Little is known about the relationship between near death experiences (NDE) and delirium. What is known is that mechanical ventilation, sedation, analgesia, primary organ dysfunction, and dissociative and spiritual propensities have been associated with the emergence of NDEs.
Case
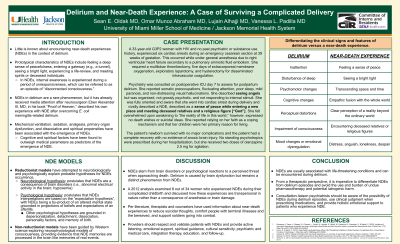
A 33-year-old G3P2 HIV-positive woman with no past psychiatric or substance use history experienced six cardiac arrests during an emergency cesarean section at 39 weeks of gestation. This occurred under general anesthesia due to right ventricular heart failure secondary to a pulmonary embolism from a suspected amniotic fluid embolism. She required multilobar thrombectomy, five days of extracorporeal membrane oxygenation (ECMO), exploratory laparotomy, and hysterectomy for disseminated intravascular coagulation (DIC). Psychiatry was consulted on postoperative ICU day seven to manage postpartum delirium. The patient reported somatic preoccupations, fluctuating attention, paranoia, and visual hallucinations. She described seeing angels but was not grossly psychotic, and not responding to internal stimuli. She was fully oriented and aware that she went into cardiac arrest during delivery and vividly described a NDE, consisting of a sense of peace while entering a new place and meeting deceased relatives and a religious figure [“God”]. She felt overwhelmed upon awakening to “the reality of life in this world,” however, expressed no death wishes or suicidal ideas. She reported relying on her faith as a coping mechanism and that her children were her primary reason for living. The patient’s newborn survived with no major complications and the patient had a complete recovery with no evidence of brain injury. No standing doses of psychotropics were prescribed, but the patient received two doses of olanzapine 2.5 mg during hospitalization.
Discussion
It has been suggested that NDEs stem from brain disorders or psychological reactions to a perceived threat when approaching death. Delirium is well-known to be caused by brain dysfunction, but remains a distinct phenomenon from NDEs. NDEs include conscious perceptual, cognitive, affective, and transcendental phenomena. Reductionist models have attempted to neurobiologically and psychologically explain probable hypotheses for NDEs occurrence. It is imperative from a therapeutic perspective to differentiate NDEs from delirium episodes and avoid the use and burden of undue pharmacotherapy and potential iatrogenic harm.
Conclusion
NDEs are usually associated with life-threatening conditions and were encountered during a delirium episode. Consultation-liaison psychiatrists should be aware of the possibility of NDE during delirium episodes, use clinical judgment when prescribing medications, and provide holistic emotional support to patients with NDE.
References
Rousseau, AF., Dams, L., Massart, Q. et al. Incidence of near-death experiences in patients surviving a prolonged critical illness and their long-term impact: a prospective observational study. Crit Care. 2023 Feb 27;27(1):76.
Facco E, Agrillo C. Near-Death-Like Experiences without Life-Threatening Conditions or Brain Disorders: A Hypothesis from a Case Report. Front Psychol. 2012 Nov 15;3:490.
Greyson B. (2013). Getting comfortable with near death experiences. An overview of near-death experiences. Missouri medicine, 110(6), 475–481.

