Trainee Involvement: Yes
- SS
Sheharyar Sarwar, DO (he/him/his)
Associate Consultant
Mayo Clinic
Rochester, Minnesota, United States .jpg)
Nicholas Allen, MD
CL Program Director
Mayo Clinic
Rochester, Minnesota, United States
Presenting Author(s)
Co-Author(s)
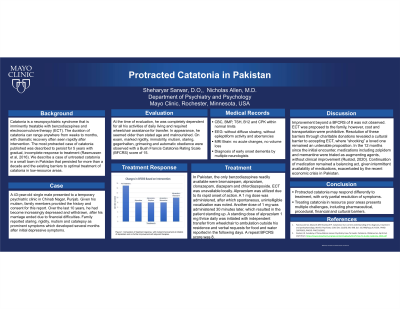
Background: Catatonia is a neuropsychiatric syndrome that is imminently treatable with benzodiazepines and electroconvulsive therapy (ECT). The duration of catatonia can range anywhere from weeks to months, with dramatic recovery often seen rapidly after intervention. The most protracted case of catatonia published was described to persist for 5 years with gradual, incomplete response to treatment (Rasmussen et al, 2016) We describe a case of untreated catatonia in a small town in Pakistan that persisted for more than a decade and the existing barriers to optimal treatment of catatonia in low-resource areas.
In Pakistan, the only benzodiazepines readily available were bromazepam, alprazolam, clonazepam, diazepam and chlordiazepoxide. ECT was unavailable locally. Alprazolam was utilized due to its rapid onset of action. A 1 mg dose was administered, after which spontaneous, unintelligible vocalization was noted. Another dose of 1 mg was administered 30 minutes later, which resulted in the patient standing up. A standing dose of alprazolam 1 mg thrice daily was initiated with independent transfer from wheelchair to ambulation outside his residence and verbal requests for food and water reported in the following days. Rasmussen SA, Mazurek MF, Rosebush PI. Catatonia: Our current understanding of its diagnosis, treatment and pathophysiology. World J Psychiatry. 2016 Dec 22;6(4):391-398. doi: 10.5498/wjp.v6.i4.391. PMID: 28078203; PMCID: PMC5183991 Rustad, JK. Academy of Consultation-Liaison Psychiatry How To Guide: Catatonia. Obtained on April 2nd, 2023 from: https://www.clpsychiatry.org/wp-content/uploads/ACLP-How-To-Guide-Catatonia-2020.pdf
Case: A 43-year-old single male presented to a temporary psychiatric clinic in Chinab Nagar, Punjab. Given his mutism, family members provided the history and consent for this report. Over the last 10 years, he had become increasingly depressed and withdrawn, after his marriage ended due to financial difficulties. Family reported staring, rigidity, mutism and catalepsy as prominent symptoms which developed several months after initial depressive symptoms. At the time of evaluation, he was completely dependent for all his activities of daily living and required wheelchair assistance for transfer. Multiple neurologists had been consulted, and reassuring brain MRI, EEG, CBC, BMP, TSH, B12 and CPK lead to a provisional diagnosis of early onset dementia. On exam, marked rigidity, immobility, mutism, staring, gegenhalten, grimacing and automatic obedience were observed with a Bush Francis Catatonia Rating Scale (BFCRS) score of 15.
Discussion: While the initial response to benzodiazepine was dramatic, with reduction in BFCRS to 8, further improvement was not observed. ECT was proposed to the family, however, cost and transportation were initially prohibitive. Resolution of these barriers through charitable donations revealed a cultural barrier to accepting ECT, where “shocking” a loved one remained an untenable proposition. In the 12 months since the initial encounter, medications including zolpidem and memantine were trialed as augmenting agents, without clinical improvement (Rustad, 2020). Continuation of medication remains a balancing act, given intermittent availability of medications, exacerbated by the recent economic crisis in Pakistan.
Conclusion: Protracted catatonia may respond differently to treatment, with only partial resolution of symptoms as demonstrated above. Treating catatonia in resource poor areas presents multiple challenges, including pharmaceutical, procedural, financial and cultural barriers.
References:

