Transplant Psychiatry
Session: Poster Session
(200) Psychiatric Considerations at Dialysis Treatment Initiation: A Case-based Discussion of Peritoneal Dialysis and Suicidal Ideation
Trainee Involvement: Yes

Morgan M. Nakatani, BA (she/her/hers)
Medical Student
Duke University
Durham, North Carolina, United States
Connie Scoggins, BS (she/her/hers)
Medical student
Duke University
Durham, North Carolina, United States
Gregg A. Robbins-Welty, MD, MS
Chief Resident, Internal Medicine & Psychiatry
Duke University Hospital
Durham, North Carolina, United States
Kristen Shirey, MD
Assistant Professor
Duke University
Durham, North Carolina, United States
Presenting Author(s)
Co-Author(s)
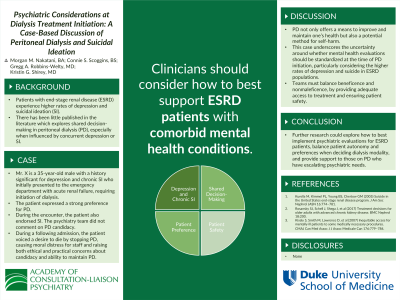
Background/Significance: Patients with end-stage renal disease (ESRD) experience higher rates of depression and suicidal ideation (SI) than the general population (Kurella, 2005). Shared decision-making is critical when helping patients with concurrent medical and psychiatric needs navigate challenging treatment decisions, including dialysis initiation. There has been little published in the literature which explores shared decision-making in peritoneal dialysis (PD), especially when influenced by concurrent depression or SI. Conclusion/Implications: CL psychiatrists should consider the challenges around how to best support ESRD patients with comorbid mental health conditions. Further research could explore how to best implement psychiatric evaluations for ESRD patients, balance patient autonomy and preferences when deciding dialysis modality, and provide support to those on PD who have escalating psychiatric needs. 1. Kurella M, Kimmel PL, Young BS, Chertow GM (2005) Suicide in the United States end-stage renal disease program. J Am Soc Nephrol JASN 16:774–781. https://doi.org/10.1681/ASN.2004070550 2. Rosansky SJ, Schell J, Shega J, et al (2017) Treatment decisions for older adults with advanced chronic kidney disease. BMC Nephrol 18:200. https://doi.org/10.1186/s12882-017-0617-3
Case: Mr. X is a 35-year-old male with a history significant for depression and chronic SI who initially presented to the emergency department (ED) with acute renal failure, requiring initiation of dialysis. The patient expressed a strong preference for peritoneal dialysis (PD) over hemodialysis, despite concerns from family members about the patient’s ability to maintain home dialysis. During the encounter, the patient also endorsed SI prompting assessment by the psychiatry team. The psychiatry team did not comment on PD candidacy. After PD initiation, the patient presented to the ED again with SI, and the team was concerned that the patient’s depression hindered his ability to complete daily PD and follow sterile technique. During a third admission, the patient presented with intractable nausea and vomiting. He voiced a desire to die by stopping PD, causing moral distress for staff and raising both ethical and practical concerns about candidacy and ability to maintain PD.
Discussion: At baseline, shared decision-making around dialysis initiation includes a discussion of the benefits, risks, and burdens of dialysis (Rosansky, 2017). In this case, the medical team needed to balance the patient’s preferences for PD with his depression and SI. Similar to many medical interventions, PD not only offers a means to improve and maintain one’s health, but also a potential method for self-harm. This case underscores the uncertainty around whether mental health evaluations should be standardized at the time of PD initiation, particularly considering the higher rates of depression and suicide in ESRD populations (Kurella, 2005). However, we must also ensure that mental health evaluations would not contribute to inequitable access to medically necessary procedures or perpetuate stigma (Kisely, 2007).
References:
3. Kisely S, Smith M, Lawrence D, et al (2007) Inequitable access for mentally ill patients to some medically necessary procedures. CMAJ Can Med Assoc J J Assoc Medicale Can 176:779–784. https://doi.org/10.1503/cmaj.060482

