Obesity, Nutrition, and Eating Disorders
Session: Poster Session
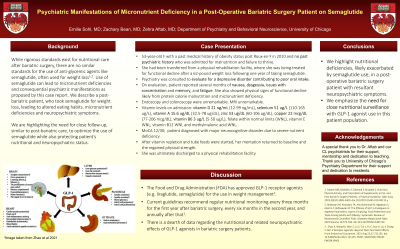
(118) Psychiatric Manifestations of Micronutrient Deficiency in a Post-Operative Bariatric Surgery Patient on Semaglutide
Trainee Involvement: Yes

Emilie Sohl, MD
Resident Physician
University of Chicago
Chicago, Illinois, United States- ZA
Zehra Aftab, MD
Assistant Professor
University of Chicago Medicine
Chicago, Illinois, United States 
Zachary Bean, MD (he/him/his)
Physician Resident
University of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Co-Author(s)
Background/Significance While rigorous standards exist for nutritional care after bariatric surgery, there are no similar standards for the use of anti-glycemic agents like semaglutide, often used for weight loss1,2. Use of semaglutide can lead to micronutrient deficiencies and consequential psychiatric manifestations as proposed by this case report. We describe a post-bariatric patient, who took semaglutide for weight loss, leading to altered eating habits, micronutrient deficiencies and neuropsychiatric symptoms. We are highlighting the need for close follow-up, similar to post-bariatric care, to optimize the use of semaglutide while also protecting patient’s nutritional and neuropsychiatric status. Case The patient is a 53-year-old woman with a past medical history of obesity status post Roux-en-Y in 2010 and no past psychiatric history who was admitted for malnutrition and failure to thrive. She had transferred from a physical rehabilitation facility, where she was being treated for functional decline after a 62-pound weight loss following one year of taking semaglutide. Psychiatry was consulted to evaluate for a depressive disorder contributing to poor oral intake. On evaluation, patient reported several months of nausea, dysgeusia, decreased interest in food, issues with concentration and memory, and fatigue. Endoscopy and colonoscopy were unremarkable. She had also functionally declined as a result of protein calorie malnutrition in the setting of micronutrient deficiencies. Her vitamin levels upon admission included: vitamin D 21 ng/mL (12-99 ng/mL), selenium 51 ug/L (110-165 ug/L), vitamin A 15.6 ug/dL (32.5-78 ug/dL), zinc 53 ug/dL (60-106 ug/dL), copper 22 mcg/dL (77-206 mcg/dL), vitamin B6 3 ug/L (5-50 ug/L), folate within normal limits (WNL), vitamin E WNL, vitamin B12 WNL and methylmalonic acid WNL. She scored 12/30 on the MoCA. Patient was diagnosed with major neurocognitive disorder due to severe nutrient deficiency. After vitamin repletion and tube feeds were started, her mentation returned to baseline and she regained physical strength. She was ultimately discharged to a physical rehabilitation facility. Discussion The Food and Drug Administration (FDA) has approved GLP-1 receptor agonists (e.g. liraglutide, semaglutide) for the use in weight management2. Current guidelines recommend regular nutritional monitoring every three months for the first year after bariatric surgery, every six months in the second year, and annually after that1. There is a dearth of data regarding the nutritional and related neuropsychiatric effects of GLP-1 agonists in bariatric surgery patients. Conclusion In this case we highlight nutritional deficiencies, likely exacerbated by semaglutide use, in a post-operative bariatric surgery patient with resultant neuropsychiatric symptoms. We emphasize the need for close nutritional surveillance with GLP-1 agonist use in this patient population. References: 1. Tabesh MR, Maleklou F, Ejtehadi F, Alizadeh Z. Nutrition, Physical Activity, and Prescription of Supplements in Pre- and Post-bariatric Surgery Patients: a Practical Guideline. Obes Surg. 2019;29(10):3385-3400. doi:10.1007/s11695-019-04112-y 2. Aldawsari M, Almadani FA, Almuhammadi N, Algabsani S, Alamro Y, Aldhwayan M. The Efficacy of GLP-1 Analogues on Appetite Parameters, Gastric Emptying, Food Preference and Taste Among Adults with Obesity: Systematic Review of Randomized Controlled Trials. Diabetes Metab Syndr Obes. 2023;Volume 16:575-595. doi:10.2147/DMSO.S387116

