Training and Education
Session: Poster Session
(195) Reproductive Psychiatry Training within C-L Psychiatry Fellowship Programs
Trainee Involvement: No

Sarah Nagle-Yang, MD
Associate Professor of Psychiatry
University of Colorado School of Medicine
Denver, Colorado, United States- WS
Whitney R. Snyders, MD
Consultation-Liaison Psychiatrist
HealthONE
Littleton, Colorado, United States - ER
Erica Rapp, MD
Assistant Professor
University of Colorado Anschutz Medical Campus
Aurora, Colorado, United States 
Lauren Osborne, MD
Vice Chair of Clinical Research, Obstetrics & Gynecology
Weill Cornell Medicine
New York, New York, United States
Presenting Author(s)
Co-Author(s)
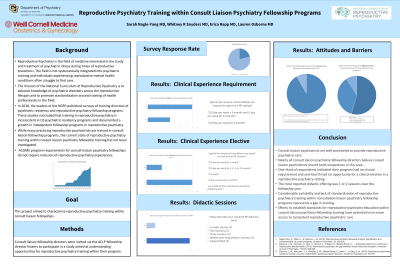
Background/Significance: Reproductive psychiatry is a rapidly developing field focused on psychiatric disorders occurring in women during periods of reproductive transition. The past decade has seen an increase in post-graduate training programs, primarily non-ACGME-accredited fellowships in reproductive psychiatry or women’s mental health. While consult-liaison (CL) psychiatry fellowship is often viewed as an additional training pathway, training in reproductive psychiatry within CL programs has not been characterized.
Methods: We invited CL fellowship directors (via ACLP listserv email) to participate in a survey about reproductive psychiatry education within their programs, including information about subspecialty track programs. The introduction email linked to the survey and stated that the survey would be summarized in an academic project. The survey was built on the Survey Monkey platform. This project was deemed exempt from IRB oversight by the Colorado Multiple Institutional Review Board.
Results: Fourteen CL fellowship directors completed the survey and were included in this study, for a response rate relative to the overall number of match-participating CL fellowship programs (n=66) of 21%. The 14 programs represented the northeast (6), southeast (2), midwest (3), mountain west (1) and west coast (2) of the US. Only one program completed questions about a subspecialty track and that information was excluded. Two-thirds (66.7%) of programs indicated they had any required clinical rotation in reproductive psychiatry, and 75% of programs reported having some elective offering. The most common clinical rotations reported were an outpatient specialty practice setting and a specialized CL inpatient service. The duration of these rotations was most commonly one half-day per week over 3-, 6- or 12- months, though one program reported a 1- day rotation over 2 months, and another reported that a fellow may elect to spend 50% of their overall time in reproductive psychiatry settings. Most (83.3%) reported offering at least one didactic session in reproductive psychiatry, most commonly 1-2 sessions across the entire fellowship year, though one program reported a weekly year-long didactic series. Notably, almost all (91.7%) fellowship directors reported that they believed that all CL psychiatrists should be competent in reproductive psychiatry. Lack of time and faculty with expertise (50% and 33.3%) were the primary barriers to incorporating more training into their program.
Discussion: CL psychiatrists are well-positioned to provide reproductive psychiatric care and nearly all CL fellowship directors believe that CL psychiatrists should hold competence in this area. However, this study found that one-third of respondents indicated their program had no requirement for a clinical offering in this field, and one-fourth had no opportunity for an elective. The most common didactic offering was 1 or 2 sessions over the entire fellowship year.
Conclusion/Implications: Considerable variability and lack of standardization of reproductive psychiatry training within CL fellowship programs represents a gap in CL fellowship training.
Nagle-Yang, et al. (2018). Reproductive psychiatry fellowship training: identification and characterization of current programs. Academic Psychiatry, 42, 202-206.
Hudepohl, et al. (2018). Advanced training in reproductive psychiatry: The case for standardization in training and a path to sub-specialty recognition. Archives of Women's Mental Health, 21, 121-123.

