Quality and Safety
Session: Poster Session
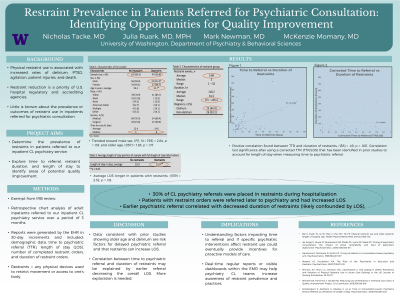
(166) Restraint Prevalence in Patients Referred for Psychiatric Consultation: Identifying Opportunities for Quality Improvement
Trainee Involvement: Yes

Nicholas Tacke, MD (he/him/his)
CL Psychiatry Fellow
Oregon Health & Science University
Portland, Oregon, United States
Julia Ruark, MD, MPH
Clinical Assistant Professor
University of Washington
Seattle, Washington, United States- MN
Mark W. Newman, MD
Clinical Associate Professor
University of Washington
Seattle, Washington, United States - MM
McKenzie Momany, MD
Psychiatry Resident
University of Washington
Seattle, Washington, United States
Presenting Author(s)
Co-Author(s)
Background:
Restraint use is associated with increased rates of delirium, PTSD, agitation, patient injuries, and death (Mitchell, 2018). In the inpatient medical setting, little is known about the prevalence or outcomes of restraint use in patients referred for psychiatric consultation. The aim of this project was to determine the prevalence of restraints in patients referred to our inpatient psychiatry consultation service. We also explored time to referral, restraint duration, and length of stay to identify areas of potential quality improvement. Methods: We performed a retrospective chart review of adult hospitalized patients referred by their primary team to our inpatient CL psychiatry service over a period of 3 months. Reports of patients referred for psychiatric consultation were generated by the electronic health record in 30-day increments and included: demographic data, time to psychiatric referral (TTR), length of stay (LOS), number of completed restraint orders, and duration of restraint orders. Restraints were any physical devices used to restrict movement or access to one’s body. Results: We received 159 general psychiatry consults over the 3-month period. Of these, 30.8% (n = 49) had completed restraint orders placed by the primary team. The median time to psychiatric referral was higher in patients with restraint orders (8 days) compared to consult patients who never had restraints (3 days). Patients with restraints trended toward older age, t(157) = 1.83, p = .07, and male sex, X2(1, N = 159) = 2.84, p = .09. 46.9% of patients with restraints were diagnosed with delirium. Average LOS was longer in consult patients who received restraints versus not, t(139) = 2.32, p = .02. A positive correlation was found between TTR and duration of restraints, r(38) = .49, p = .001, though this lost statistical significance when adjusting for LOS. Discussion: Patients with restraint orders trended older, were referred later to psychiatric consultation, and had increased LOS. This is consistent with prior studies showing older age and delirium are risk factors for delayed psychiatric referral and that restraints can increase LOS (Bai, 2014; de Jonge, 2000). Our correlation between time to psychiatric referral and duration of restraints may be explained by earlier referral decreasing the overall LOS, though more exploration is needed (Sockalingam, 2016). Conclusion/Implications: Restraints were frequently encountered by our inpatient consultation service. Understanding factors impacting time to referral and if specific psychiatric interventions affect restraint use could eventually provide incentives for proactive models of care. References: Bai X, Kwok TC, Ip IN, Woo J, Chui MY, Ho FK. Physical restraint use and older patients' length of hospital stay. Health Psychol Behav Med. 2014;2(1):160-170. de Jonge P, Huyse FJ, Ruinemans GM, Stiefel FC, Lyons JS, Slaets JP. Timing of psychiatric consultations: the impact of social vulnerability and level of psychiatric dysfunction. Psychosomatics. 2000;41(6):505-511. Mitchell DA, Panchisin T, Seckel MA. Reducing Use of Restraints in Intensive Care Units: A Quality Improvement Project. Crit Care Nurse. 2018;38(4):e8-e16. Sockalingam S, Alzahrani A, Meaney C, et al. Time to Consultation-Liaison Psychiatry Service Referral as a Predictor of Length of Stay. Psychosomatics. 2016;57(3):264-272.

