Substance Use and Related Disorders
Session: Poster Session
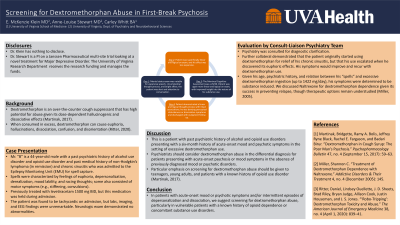
(171) Screening for Dextromethorphan Abuse in First-Break Psychosis
Trainee Involvement: Yes

Elizabeth McKenzie Klein, MD
Resident Physician
University of Virginia
Charlottesville, Virginia, United States- AS
Anne Louise Stewart, MD
Assistant Professor of Psychiatry
University of Virginia
Charlottesville, Virginia, United States - CW
Carley C. Whitt, n/a
Medical student
University of Virginia School of Medicine
Charlotteville, Virginia, United States
Presenting Author(s)
Co-Author(s)
Elizabeth McKenzie Klein MD, Anne Louise Stewart MD, Carley Whitt
Background/Significance
Dextromethorphan is an over-the-counter cough suppressant that has high potential for abuse given its dose-dependent hallucinogenic and dissociative effects (Martinak, 2017). When consumed in excess, dextromethorphan can cause euphoria, hallucinations, dissociation, confusion, and disorientation (Ritter, 2020).
Case
Mr. “B” is a 44-year-old male with a past psychiatric history of alcohol use disorder and opioid use disorder and past medical history of non-Hodgkin’s lymphoma (in remission) and chronic sinusitis who was admitted to the Epilepsy Monitoring Unit (EMU) for spell capture. The patient’s spells were characterized by feelings of euphoria, depersonalization, derealization, mood lability, and racing thoughts; some spells also consisted of motor symptoms (e.g., stiffening, convulsions). The patient had been prescribed levetiracetam 1500 mg BID, which was held during admission. The patient was found to be tachycardic on admission, but labs, imaging, and EEG findings were unremarkable. Neurologic exam demonstrated no abnormalities. Psychiatry was consulted for diagnostic clarification. Psychiatric exam was notable for expansive speech, circumstantial thought process, and bright affect; the patient was alert and attentive to conversation. Notably, his expansive speech and disorganized thought process improved over admission. The Montreal Cognitive Assessment was a 29/30. Further collateral demonstrated that the patient originally started using dextromethorphan for relief of his chronic sinusitis, but that his use escalated when he discovered its euphoric effects. Moreover, his symptoms would improve and recur with reuse. Given his age, psychiatric history, and relation between his “spells” and excessive dextromethorphan ingestion (up to 1422 mg/day), his symptoms were determined to be substance induced. We discussed Naltrexone for dextromethorphan dependence given its success in preventing relapse, though therapeutic options remain understudied (Miller, 2005). Discussion This is a patient with past psychiatric history of alcohol and opioid use disorders presenting with a six-month history of acute-onset mood and psychotic symptoms in the setting of excessive dextromethorphan use. Psychiatrists should consider dextromethorphan abuse in the differential diagnosis for patients presenting with acute-onset psychosis or mood symptoms in the absence of previously diagnosed mood or psychotic disorders. Particular emphasis on screening for dextromethorphan abuse should be given to teenagers, young adults, and patients with a known history of opioid use disorder (Martinak, 2017). Conclusion/Implications In patients with acute-onset mood or psychotic symptoms and/or intermittent episodes of depersonalization and dissociation, we suggest screening for dextromethorphan abuse, particularly in vulnerable patients with a known history of opioid dependence or concomitant substance use disorders. References [1] Martinak, Bridgette, Ramy A. Bolis, Jeffrey Ryne Black, Rachel E. Fargason, and Badari Birur. “Dextromethorphan in Cough Syrup: The Poor Man’s Psychosis.” Psychopharmacology Bulletin 47, no. 4 (September 15, 2017): 59–63. [2] Miller, Shannon C. “Treatment of Dextromethorphan Dependence with Naltrexone.” Addictive Disorders & Their Treatment 4, no. 4 (December 2005): 145. [3] Ritter, Daniel, Lindsey Ouellette, J. D. Sheets, Brad Riley, Bryan Judge, Allison Cook, Justin Houseman, and J. S. Jones. “‘Robo-Tripping’: Dextromethorphan Toxicity and Abuse.” The American Journal of Emergency Medicine 38, no. 4 (April 1, 2020): 839–41.

