COVID-19
Session: Poster Session
(066) "She Needs to Die": Seronegative Autoimmune Encephalitis after COVID-19 Infection Presenting as Homicidal Ideation
Trainee Involvement: Yes
- TS
Todd Stollenwerk, PhD
Medical Student
Medical College of Wisconsin
Milwaukee, Wisconsin, United States 
Ana M. Navarro-Montoya, MD
Assistant Professor
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Co-Author(s)
Introduction
Autoimmune encephalitis is an immune-mediated disorder characterized by neuroinflammation and neuropsychiatric symptoms secondary to antibodies against neuronal cell surface proteins, ion channels, or receptors1. Growing evidence suggests that COVID-19 infection can cause autoimmune encephalitis2. We describe a previously unreported case of seronegative autoimmune encephalitis following COVID-19 infection manifesting as homicidal ideation in the context of delusions.
Case Presentation
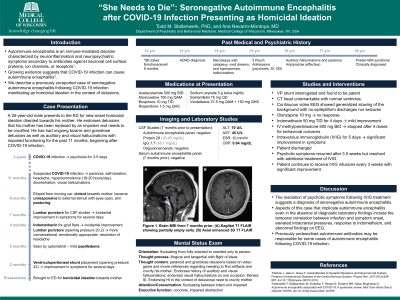
A 25-year-old male with a history of TBI, narcolepsy (treated with atomoxetine), REM sleep behavior disorder with status dissociatus (treated with sodium oxybate), and prior psychosis (previously stable on risperidone) presented to the ED for new-onset homicidal ideation directed towards his mother based in delusions that his mother had been replaced by an imposter and needed to be crucified. He had ongoing delusions of grandiosity and auditory and visual hallucinations with impaired functioning for 11 months, beginning after COVID-19 infection. He also had an episode of psychosis lasting for 3-5 days after a first COVID-19 infection 10 months prior to most recent infection.
Earlier during this episode, neuroimmune workup was negative (negative CSF and serum autoimmune encephalopathy panels; no elevation of CSF protein or IgG). However, there was transient improvement in symptoms following lumbar punctures and indomethacin treatment (given incidentally for gout). He had a ventriculoperitoneal shunt placement 2 months before current admission with elevated opening pressure, which resulted in transient improvement of symptoms lasting several days. Multiple changes in antipsychotic drugs during this prolonged period of psychosis were ineffective.
During the current hospitalization, continuous EEG showed generalized slowing of the background with no epileptiform discharges nor seizures. All other imaging and metabolic and infectious labs were unremarkable. There was mild improvement following indomethacin treatment (50 mg TID for 4 days). He was started on IV methylprednisolone 500 mg BID to treat empirically for autoimmune encephalitis, which was stopped after 4 doses for behavioral concerns. The patient received a 5-day course of intravenous immunoglobulin (IVIG), resulting in improvement in psychosis sufficient for discharge. Following discharge, psychosis returned but was successfully treated with outpatient IVIG infusions.
Discussion
The resolution of psychotic symptoms following IVIG treatment suggests a diagnosis of seronegative autoimmune encephalitis in this case. Several cases of autoimmune encephalitis have been reported following COVID-19 infections2. Aspects of this case that implicate autoimmune encephalitis even in the absence of diagnostic laboratory findings include the temporal correlation between infection and symptom onset, elevated intracranial pressures, response to indomethacin, and abnormal findings on EEG. This suggests that previously undescribed autoimmune antibodies may be responsible for some cases of autoimmune encephalitis following COVID-19 infection.
Conclusion
New-onset or worsening psychosis following COVID-19 infection may be successfully treated with IVIG, even in the absence of laboratory findings suggestive of autoimmune encephalitis.
References
1Dalmau J, Geis C, Graus F. Autoantibodies to Synaptic Receptors and Neuronal Cell Surface Proteins in Autoimmune Diseases of the Central Nervous System. Physiol Rev. 2017;97(2):839-887. doi:10.1152/physrev.00010.2016.
2Nabizadeh F, Balabandian M, Sodeifian F, Rezaei N, Rostami MR, Naser Moghadasi A. Autoimmune encephalitis associated with COVID-19: A systematic review. Mult Scler Relat Disord. 2022;62:103795. doi:10.1016/j.msard.2022.103795

