Diversity, Equity, and Inclusion
Session: Poster Session
(073) Social Determinants of Health & Why They Matter to C-L Psychiatry
Trainee Involvement: Yes

Nicholas Flugrad, MD (he/him/his)
Psychiatry Resident, Department of Psychiatry Jersey Shore University Medical Center
Hackensack Meridian Healthcare Network
neptune, New Jersey, United States- ET
Eamon Thomasson, M.D.
Psychiatry Resident, Department of Psychiatry Jersey Shore University Medical Center
Hackensack Meridian Healthcare Network
Neptune, New Jersey, United States
Presenting Author(s)
Co-Author(s)
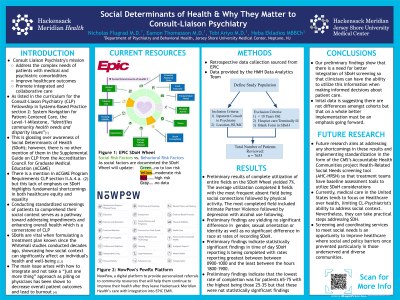
Consult-Liason Psychiatry's mission is to address the complex needs of patients with medical and psychiatric comorbidities, improve healthcare outcomes, and promote integrated and collaborative care. As listed in the curriculum for the Consult-Liason (CL) Psychiatry Fellowship in Systems-Based Practice section 2: System Navigation for Patient-Centered Care, the Level-1-Milestone, “Identifies community health needs and disparity issues”[1]. This glosses over awareness of Social Determinants of Health (SDOH); however, there is no other mention of them in the Supplemental Guide on CL-Psychiatry from the Accreditation Council for Graduate Medical Education (ACGME). There is a mention in ACGME Program Requirements CL-Psychiatry section-II.A.4.a.(2); however, this lack of emphasis on SDOH highlights fundamental shortcomings in both healthcare equity and equality. Conducting standardized screenings of patients to comprehend their social context serves as a pathway toward addressing impediments and enhancing overall health which is a cornerstone of CL-Psychiatry. SDOHs are a vital component taken into consideration when formulating a treatment plan. This has been a known consensus since the Whitehall studies conducted decades ago, showcased how social context can significantly affect an individual's health and well-being [2,3]. The main issue arises with how to integrate this imperative information and obtain it in the first place. The aim is to not take a “just one more thing” approach as piling on physicians has been shown to decrease overall patient outcomes and lead to burnout [4]. Instead, the better approach is a collaborative stance utilizing the entire treatment team. Screening for SDOHs differs fundamentally from conventional medical screening. Nonetheless, both necessitate screening in an environment where suitable referral or connection to resources to tackle a recognized need can be established. This research aims to quantify SDOH screening of CL-Psychiatry at a Teaching Hospital, assessing the rates and analyzing for disparities. Utilizing a retrospective chart review from (01/01/2020-01/01/2023) demographic factors, primary-diagnosis were evaluated, and overall patient outcomes compared with SDOH rates. Descriptive statistics were reported from the data. Categorical data were reported as proportions and percentages, counts and score-type data were reported as medians and ranges, and quantitative data was reported as means and standard deviations. Cross-tabulations between variables such as demographic factors, clinical diagnoses, and patient outcomes, were quantified and analyzed using Chi-square, Fisher’s exact tests, t-tests, ANOVA, quantile regression, or generalized linear models. Differences where P< 0.05 were considered statistically significant and reported as differences between groups fold differences or odds ratios with 95% CI. Future research aims at addressing any shortcomings in these results and implementing standardization in the form of the CMS’s Accountable Health Communities project Health-Related Social Needs screening tool (AHC-HRSN) so that treatment teams have baseline assessment tools to utilize SDOH considerations. Currently, medical care in the United States tends to focus on Healthcare over health, limiting CL-Psychiatrist's ability to address social context. Nevertheless, they can take practical steps addressing SDOH. Screening and coordinating services to meet social needs is an opportunity to improve healthcare where social and policy barriers once prevented particularly in those underserved and diverse communities.
1.The.Accreditation.Council.for.Graduate.Medical.Education.(2022).Consultation-Liaison.Psychiatry.Milestones:The.Accreditation.Council.for.Graduate.Medical.Education.Implementation:July.2022.Second.Revision:.August.2021.First.Revision:.September.2014.Retrieved.January2,2023,from.https://www.acgme.org/globalassets/pdfs/milestones/consultationliaisonpsychiatrymilestones.pdf
2.Marmot.MG,Rose.G,Shipley.M,Hamilton.PJ.Employment.grade.and.coronary.heart.disease.in.British.civil.servants.J.Epidemiol.Community.Health.(1978).1978.Dec;32(4):244-9.doi:10.1136/jech.32.4.244.PMID:744814;PMCID:PMC1060958.
3.Marmot.MG,Smith.GD,Stansfeld.S,Patel.C,North.F,Head.J,White.I,Brunner.E,Feeney.A.Health.inequalities.among.British.civil.servants:the.Whitehall.II.study.Lancet.1991.Jun 8;337(8754)1387-93.doi:10.1016/0140-6736(91)93068-k.PMID:1674771.
4.Patel.RS,Bachu.R,Adikey.A,Malik.M,Shah.M.Factors.Related.to.Physician.Burnout.and.Its.Consequences:A.Review.Behav.Sci(Basel).2018.Oct.25;8(11):98.doi:10.3390/bs8110098.PMID:30366419;PMCID:PMC6262585.

