COVID-19
Session: Poster Session
(063) Somatic Symptoms and Associated Psychological Perceptions Among Patients With and Without Post-acute Sequalae of SARS-CoV-2 and Controls
Trainee Involvement: Yes
- ML
Michael R. Liu, B.S.
Research Assistant
National Institute of Mental Health
Rockville, Maryland, United States 
Haniya Raza, DO
Chief, Psychiatry Consultation Liaison Service
National Institute of Mental Health
Bethesda, Maryland, United States- EG
Emily P. Guinee, B.S.
Postbaccalaureate Intramural Research Training Award
National Institute of Mental Health
Washington, District of Columbia, United States - MS
Michael Sneller, MD
Medical Officer
National Institute of Allergy and Infectious diseases
Bethesda, Maryland, United States .jpg)
Joyce Chung, MD
Executive Director, Graduate Medical Education & Designated Institutional Official
National Institutes of Health Clinical Center
Bethesda, Maryland, United States
Presenting Author(s)
Co-Author(s)
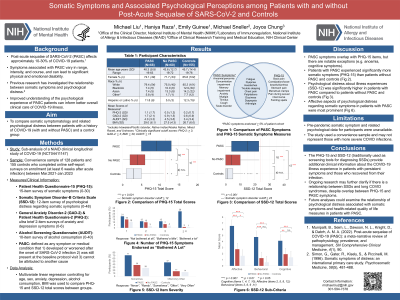
Background: Post-acute sequelae of SARS-CoV-2 (PASC), characterized by persistent clinical symptoms four weeks after the onset of the acute infection, affect approximately 10-30% of patients (Munipalli et al., 2022). PASC symptoms are variable and can lead to significant physical and emotional difficulties. There is a relationship between severity of somatic symptoms and psychological distress (Simon et al., 1996). The aim of this study is to compare responses to measures of somatic symptoms and psychological perceptions of symptoms among patients with history of COVID-19 (with/without PASC) and controls.
Methods: This is a sub-analysis of a longitudinal study of the medical sequelae of COVID-19, conducted by the National Institute of Allergy and Infectious Diseases (NCT04411147). Patients and controls who enrolled between March 2021-August 2022 completed the Patient Health Questionnaire-15 (PHQ-15) and the Somatic Symptom Disorder – B Criteria Scale (SSD-12), which assess clinical severity of somatic symptoms and associated psychological distress, respectively. Using multivariate linear regression (controlling for age, sex, race, BMI, PHQ-2, GAD-2), PHQ-15 and SSD-12 total scores were compared between controls and patients with and without PASC. The most frequent items endorsed on the PHQ-15 and SSD-12 will be determined for each group. Individual items on the PHQ-15 and SSD-12 will be analyzed according to score severity among groups.
Munipalli, B., Seim, L., Dawson, N. L., Knight, D., & Dabrh, A. M. A. (2022). Post-acute sequelae of COVID-19 (PASC): a meta-narrative review of pathophysiology, prevalence, and management. SN Comprehensive Clinical Medicine, 4(1), 90. Nalbandian, A., Sehgal, K., Gupta, A., Madhavan, M. V., McGroder, C., Stevens, J. S., ... & Wan, E. Y. (2021). Post-acute-COVID-19 syndrome. Nature medicine, 27(4), 601-615. Simon, G., Gater, R., Kisely, S., & Piccinelli, M. (1996). Somatic symptoms of distress: an international primary care study. Psychosomatic medicine, 58(5), 481-488.
Results: The study sample consisted of 255 participants (128 patients; 127 matched controls). Of the 128 patients, 66 (52%) had PASC. Compared to controls, patients with PASC reported statistically significantly higher PHQ-15 scores (β = 4.09, 95% CI = 2.99-5.21, p < 0.001). There was no significant difference in PHQ-15 scores between patients without PASC and controls (β = 0.578, 95% CI = -0.268-1.42, p = 0.182). Total SSD-12 scores were significantly higher in both patient groups compared to controls [PASC: β = 7.76, 95% CI = 5.46-10.05, p < 0.001; no PASC: β = 3.45, 95% CI = 0.60-4.13, p = 0.009]. Additional analysis is in progress.
Discussion: Patients with PASC reported significantly higher rates of somatic symptoms and psychological distress regarding their symptoms, supporting existing research that patients who have persistent COVID-19 symptoms experience heightened psychological distress (Nalbandian et al., 2021).
Conclusion: The PHQ-15 and SSD-12 may be useful measures to understand the COVID-19 illness experience. PASC are associated with a multitude of potentially debilitating symptoms including depression and anxiety. Current guidelines recommend a multidisciplinary approach, including mental health care, in the management of post-COVID-19 syndrome. Consult-liaison psychiatrists may lend additional expertise in the management of psychological distress in the context of persistent somatic symptoms.
References:

