Psycho-Oncology and Palliative Care
Session: Poster Session
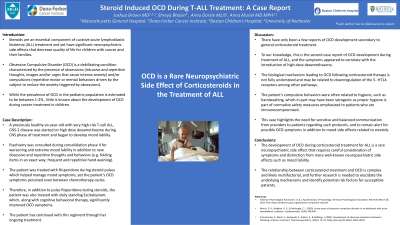
(122) Steroid Induced OCD during T-ALL Treatment: A Case Report
Trainee Involvement: No

Joshua Brown, MD
Attending Physician
Massachusetts General Hospital; Harvard Medical School; Dana-Farber Cancer Institute;
Cambridge, Massachusetts, United States
Shreya Bhasin, BA
Medical Student
University of Rochester School of Medicine and Dentistry
Rochester, New York, United States
Anna Dorste, MLIS
Medical Librarian
Boston Children's Hospital Medical Library
Boston, Massachusetts, United States.jpg)
Anna Muriel, MD, MPH
Division Chief, Pediatric Psychosocial Oncology
Dana Farber Cancer Institute
Boston, Massachusetts, United States
Presenting Author(s)
Co-Author(s)
Background:
Steroids are an essential component of curative acute lymphoblastic leukemia (ALL) treatment and yet have significant neuropsychiatric side effects that decrease quality of life for children with cancer and their families. Obsessive Compulsive Disorder (OCD) is a debilitating condition characterized by the presence of obsessions (intrusive and repetitive thoughts, images and/or urges that cause intense anxiety) and/or compulsions (repetitive motor or mental behaviors driven by the subject to reduce the anxiety triggered by obsessions).1 While the prevalence of OCD in the pediatric population is estimated to be between 1-2%1, little is known about the development of OCD during cancer treatment in children. Patient is a previously healthy six-year-old with very high-risk T-cell ALL, CNS-2 disease. The patient was started on high dose dexamethasone during CNS phase of treatment and began to develop mood lability. Psychiatry was consulted during consolidation phase II for worsening and extreme mood lability in addition to new obsessive and repetitive thoughts and behaviors (e.g. folding items in an exact way; frequent and repetitive hand washing). The patient was treated with Risperidone during steroid pulses which helped manage mood symptoms, yet the patient’s OCD symptoms persisted even between chemotherapy cycles. Therefore, in addition to the Risperidone, the patient was also treated with daily standing Escitalopram, which, along with cognitive behavioral therapy, significantly improved OCD symptoms. There have only been a few reports of OCD development secondary to corticosteroid treatment.2 3 To our knowledge, this is the second case report of OCD development during treatment of ALL, and the symptoms appeared to correlate with the introduction of high dose dexamethasone. The biological mechanism leading to OCD following corticosteroid therapy is not fully understood and may be related to downregulation of the 5-HT1A receptors among other pathways.3 The patient’s compulsive behaviors were often related to hygiene, such as handwashing, which in part may have been iatrogenic as proper hygiene is part of normative safety measures emphasized to patients who are immunocompromised. This case highlights the need for sensitive and balanced communication from providers to patients regarding such protocols, and to remain alert for possible OCD symptoms in addition to mood side effects related to steroids. The development of OCD during corticosteroid treatment for ALL is a rare neuropsychiatric side effect that requires careful consideration of symptoms and distinction from more well-known neuropsychiatric side effects such as mood lability. The relationship between corticosteroid treatment and OCD is complex and likely multifactorial, and further research is needed to elucidate the underlying mechanisms and identify potential risk factors for susceptible patients. 1American Psychological Association. (n.d.). Apa Dictionary of Psychology. American Psychological Association. Retrieved March 28, 2023, from https://dictionary.apa.org/obsessive-compulsive-disorder 2 Morris, D. R., Meighen, K. G., & Mcdougle, C. J. (2005). Acute onset of obsessive-compulsive disorder in an adolescent with acute lymphoblastic leukemia. Psychosomatics, 5(46), 458-460 3Scheschonka, A., Bleich, S., Buchwald, A., Ruther, E., & Wiltfang, J. (2002). Development of obsessive-compulsive behaviour following cortisone treatment. Pharmacopsychiatry, 35(02), 72–74. https://doi.org/10.1055/s-2002-25022
Case Description:
Discussion:
Conclusion:
References:

