Child and Adolescent Psychiatry
Session: Poster Session
(040) Synthetic Cannabis induced Agitated Catatonia in Adolescents
Trainee Involvement: Yes

Raheel Chaudhry, MD
Physician
Doctor on Demand
Houston, Texas, United States- SN
Sohail Nibras, MD
Assistant Professor
Baylor College Of Medicine
Houston, Texas, United States
Presenting Author(s)
Co-Author(s)
2.Yeruva, R., S. (2019). Synthetic Cannabinoids—” Spice” Can Induce a Psychosis: A Brief Review. Innovations in clinical neuroscience, 16(1-2), 31. 3.10.7759/cureus.8603 4.https://doi.org/10.1111/ajad.12318 5.https://doi.org/10.1080/15504263.2021.1904163
Background:
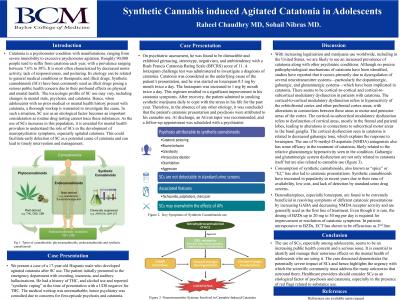
Catatonia is a psychomotor condition with manifestations, ranging from severe immobility to excessive psychomotor agitation. The toxicologic profile of Synthetic Cannabinoid(SC) use may vary, including changes in mental state, psychosis, and catatonia. SC use as an etiological factor becomes an important consideration as routine drug testing cannot trace these substances. As the use of SCs increases in this population, it is essential for mental health providers to understand the role of SCs in the development of neuropsychiatric symptoms, especially agitated catatonia.
Methods:
We present a case of a 17-year-old Hispanic male who developed agitated catatonia after SC use. The patient initially presented to the emergency department with sweating, insomnia, and auditory hallucinations. He had a history of THC, and alcohol use and reported “synthetic vaping” at the time of presentation with a UDS positive for THC. The workup was unremarkable; hence psychiatry was consulted due to concerns about first-episode psychosis and catatonia. On psychiatric assessment, he was found to have catatonia with a Bush Francis Catatonia Rating Scale (BFCRS) score of 11. He was scheduled on oral clonazepam with a subsequent reduction in the BFCRS score to 9. He continued to improve over the course of hospitalization with some residual disorganized thought processes. Inpatient psychiatric hospitalization was offered but parents opted for outpatient care. Clonazepam taper was recommended and a follow-up appointment was scheduled with a psychiatrist.
Discussion:
Through this case report we will present the case and provide the timeline and clinical management. We will expand upon possible SC-related psychiatric symptoms which may include anxiety, paranoia, agitation, confusion, as well as catatonia as noted in the cases under discussion. We will explore the relationship of SC use with catatonic symptoms in the adolescent population. As in our case report, benzodiazepines are shown to not only validate the diagnosis of catatonia but are also the mainstay for the management of catatonia. We will discuss the management of catatonia in adolescents with SC use. We will discuss the challenges associated with identifying the etiology of catatonia in the adolescent population, particularly given that SC are not detected on traditional UDS.
Conclusions:
The use of SCs, especially among adolescents, seems to be an increasing public health concern and a serious issue. It is essential to identify and manage their notorious effects on the mental health of adolescents who are using it. The cases discussed to demonstrate the potentially severe impact of SCs and hence highlight the urgency with which the scientific community must address the many unknowns that surround them. Healthcare providers should consider SCs as an etiological factor of AMS and catatonia, especially in the presence of red flags related to substance use.
References:
1.Khan, M., Pace, L., Truong, A., Gordon, M., & Moukaddam, N. (2016). Catatonia secondary to synthetic cannabinoid use in two patients with no previous psychosis. The American journal on addictions, 25(1), 25-27.

