Psychopharmacology and Toxicology
Session: Poster Session
(140) Tears Without Fears: Psychopharmacologic Considerations When Treating Pseudobulbar Affect
Trainee Involvement: Yes
.jpg)
Jacob Cross, MD (he/him/his)
Resident Physician
Rush University Medical Center
Chicago, Illinois, United States- AO
Andrew Oreshkov, MD Candidate
Medical Student
Rush University Medical Center
Chicago, Illinois, United States - JE
Joshua Eloge, MD
Assistant Professor of Psychiatry and Behavioral Sciences
Rush University Medical Center
Chicago, Illinois, United States
Presenting Author(s)
Co-Author(s)
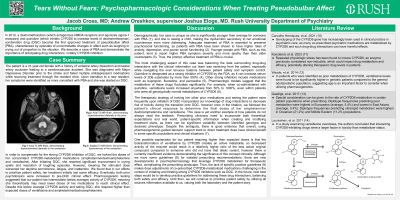
In 2010, the dextromethorphan (which antagonizes NMDA receptors and agonizes sigma-1 receptors) and quinidine (which inhibits CYP2D6 to increase levels of dextromethorphan) combination drug (DQC) became the first approved treatment of pseudobulbar affect (PBA), characterized by episodes of uncontrollable changes in affect such as laughing or crying out of proportion to the situation. We describe a case of PBA and demonstrate the importance of anticipating drug interactions, notably CYP2D6 inhibition. Case Summary The patient is a 31-year-old female with a history of vertebral artery dissection and basilar artery occlusion leading to a cerebrovascular accident. She was also diagnosed with Major Depressive Disorder prior to the stroke but had not responded to multiple antidepressant medications while receiving treatment through the resident clinic. Upon transition to a new resident, the clinical signs of her emotional incontinence were identified as more consistent with PBA and she was started on DQC. To compensate for the CYP2D6 inhibition of DQC, the doses of her concomitant 2D6-metabolized medications (amphetamine/dextroamphetamine and venlafaxine) were halved. She reported significant improvement in crying spells and resolution of laughing episodes. However, lowering her amphetamine/dextroamphetamine worsened daytime somnolence, fatigue, and inattention. Both preceding psychotropics were increased to pre-DQC clinical effect. Ultimately, she required higher than originally expected doses of venlafaxine and amphetamine/dextroamphetamine. Discussion Several elements in this case are noteworthy. One unique opportunity in the resident clinic is the regular transitions of care that facilitate scrutiny of prior diagnoses and avoidance of diagnostic overshadowing. This patient had not responded to previous treatments targeting a diagnosis that preceded her stroke, but did respond to a medication that would not have been utilized if an alternative diagnosis was not considered. Her life stage is important as she was raising a young child, making the dysfunction secondary to her emotional incontinence even more distressing. Adequate treatment of PBA is essential to preserve psychosocial functioning, as this diagnosis is associated with higher rates of anxiety, depression, and poorer social functioning (Tateno, 2004). Younger people with PBA, such as this patient, tend to report higher PBA severity and more apathy than their older counterparts (Patel, 2018). Recent developments in psychopharmacology leverage CYP2D6 metabolism, but a lack of specific practice guidelines makes dose adjustments of co-prescribed CYP2D6-metabolized medications challenging. Here, we present an approach that prioritizes safety in adjusting other CYP2D6 substrates and discuss additional considerations for the prescribing clinician. Implications - Identification of risk factors can facilitate screening and treatment of PBA - Consider using our treatment algorithm if patient is already taking 2D6 substrates when initiating DQC - Future directions should include best practice guidelines for addressing drug interactions References 1) Tateno, A., Jorge, R. E., & Robinson, R. G. (2004). Pathological laughing and crying following traumatic brain injury. The Journal of neuropsychiatry and clinical neurosciences, 16(4), 426–434.
Background
2) Patel, N., Combs, H., York, M., Phan, C., & Jimenez-Shahed, J. (2018). Pseudobulbar Affect Correlates With Mood Symptoms in Parkinsonian Disorders but Not Amyotrophic Lateral Sclerosis. The Journal of neuropsychiatry and clinical neurosciences, 30(3), 214–219.

