Neurocognitive Disorders, Delirium, and Neuropsychiatry
Session: Poster Session
(083) "TEMP"orarily Missed: A Case of Temporal Lobe Epilepsy Complicated by Hyperactive Catatonia
Trainee Involvement: No
- AS
Anna P. Shapiro-Krew, MD
CL Psychiatry Associate Staff, Associate Program Director for CL Fellowship
Cleveland Clinic
Cleveland, Ohio, United States - NB
Nora K. Burns, DO
Staff Psychiatrist
Cleveland Clinic Foundation
Lakewood, Ohio, United States
Presenting Author(s)
Co-Author(s)
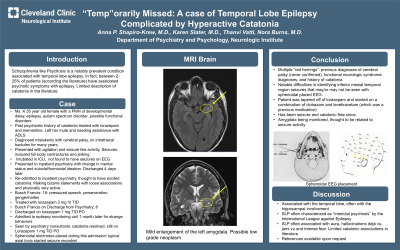
Schizophrenia like psychosis (SLP) is a well documented phenomenology that occurs in patients with intractable epilepsy, particularly temporal lobe epilepsy (1.) However, reports of this phenomenology have indicated limited evidence of catatonic features (1.) We presented case of a young woman who was having undiagnosed inferior temporal seizures and hyperactive catatonia. Ms. K was a 35-year-old female with a history of cerebral palsy, epilepsy, PEG tube feedings, autism spectrum disorder, and suspected psychogenic nonepileptic seizures. She had a history of catatonia 15 years before admission and had received ECT and was placed in a nursing facility for 3 months. At that time, she was also tried on memantine. Patient initially presented to our medical facility for seizure activity as well as agitated behaviors. After several days of electroencephalogram placement, no seizures were recorded. Behaviors were thought to be related to stress and patient was discharged. Two days later, she was admitted to inpatient psychiatry. She presented with worsening suicidal/homicidal ideation and bizarre, disorganized, psychotic behaviors. She was very aggressive initially threatening to "smack" care providers. On initial examination her Bush Francis Catatonia Rating Score (BFCRS) was 18 and was notable for pressured speech, perseveration and gegenhalten. She was diagnosed with excited catatonia. During hospitalization she received doses of lorazepam up to 2 mg IV 3 times daily. MRI was notable for left amygdala enlargement and low-grade neoplasm, although this was seen previously. She was discharged on 1 mg of lorazepam 3 times daily PO (BFCRS-6) and levetiracetam. One month after psychiatric admission, she was admitted to the epilepsy monitoring unit during for continued video EEG monitoring, due to continued concern for seizure like episodes and strange behaviors. During this admission sphenoidal electrodes were placed and several typical axial tonic startle seizures were recorded due to the sphenoidal placement of the leads. Following the discovery of tonic seizures, patient was placed on combination of clobazam and levetiracetam. Patient appeared calm and cooperative during hospitalization and did not appear to have significant catatonic symptomatology. She was slowly weaned off lorazepam over the course of 3 weeks. Patient was seen as an outpatient 2 months following hospitalization and remained symptom free of catatonia. After patient's initial EEG was negative, there was thought that convulsive events were related to a psychogenic nonepileptic syndrome with a relationship to psychosis. However, after the introduction of the EEG with sphenoidal electrodes (which measured the inferior mesial temporal region), it was clear that patient was experiencing significant electrical activity in the temporal lobes that may have resulted in catatonic symptomatology. The relationship between epilepsy and psychiatric comorbidities, such as catatonia, still requires significant elucidation. This case advocates for aggressive neurologic workup in patients with sudden/unexplained psychiatric symptoms and a history of epilepsy. Sources:
Introduction:
Case:
Discussion:
1. Adachi N, Onuma T, Nishiwaki S, Murauchi S, Akanuma N, Ishida S, Takei N. Inter-ictal and post-ictal psychoses in frontal lobe epilepsy: a retrospective comparison with psychoses in temporal lobe epilepsy. Seizure. 2000 Jul;9(5):328-35

