Psychopharmacology and Toxicology
Session: Poster Session
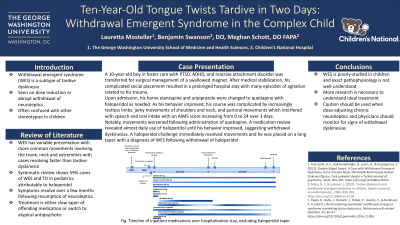
(143) Ten-Year-Old Tongue Twists Tardive in Two Days: Withdrawal Emergent Syndrome in the Complex Child
Trainee Involvement: Yes

Lauretta Mosteller (she/her/hers)
Medical Student
The George Washington University
Arlington, Virginia, United States
Benjamin Swanson, DO
CAP Fellow
Children's National Hospital
Washington, District of Columbia, United States
Meghan Schott, DO FAPA
Medical Director of Psychiatric Emergency Services
Children's National
Washington, District of Columbia, United States
Presenting Author(s)
Co-Author(s)
Background: Withdrawal emergent syndrome (WES) is a subset of tardive dyskinesia (TD) seen on dose reduction or abrupt withdrawal of neuroleptic medications and is poorly-studied in children. The syndrome is furthermore difficult to diagnose, with movements often confused for stereotypies seen in other psychiatric disorders for which the neuroleptics are prescribed.
Case: Juan is a 10-year-old male in foster care with PTSD, ADHD and reactive attachment disorder who was transferred from an outside hospital for emergent surgical care after swallowing a magnet while awaiting psychiatric treatment. After medical stabilization, it was determined he did not need inpatient stabilization as he was at his baseline. However, due to being a ward of a different state, he remained in the inpatient medical unit with episodes of agitation related to his trauma requiring medication adjustments. He was admitted on olanzapine and aripiprazole which were replaced with quetiapine with haloperidol as needed for agitation. As his behavior improved, his course was complicated by increasingly restless limbs, jerky movements of his shoulders and neck as well as perioral movements interfering with his movement, speech, and oral intake. This notably worsened after administration of quetiapine. On further review, his improving behaviors had eliminated haloperidol use which had been used almost daily. He was given a trial of haloperidol with immediate resolution. Patient was diagnosed with WES following abrupt discontinuation of haloperidol. Quetiapine was stopped, and the patient was started on a long taper of haloperidol which he tolerated well with no recurrence of WES.
Discussion: WES presentation varies widely, but movements more commonly involve the trunk, neck and extremities and resolve sooner than TD, though the behavior often looks quite similar. A systematic review of pediatric cases of TD and WES demonstrated 59% of observed WES cases were attributable to haloperidol, though it has also been reported in atypical antipsychotics and metoclopramide (Mejia, 2010). Cases typically resolve over a couple months with neuroleptic resumption expediting recovery (Pugin, 2017). There is, however, no consensus on treatment of WES; common approaches either restart the original medication to slow taper or switch to an atypical antipsychotic with lower dopamine receptor affinity (Arat-Çelik, 2021).
Conclusion: More research is needed to understand the pathophysiology of WES and its ideal treatment, especially in children, and providers should be urged to be cautious dose-adjusting chronic neuroleptics while monitoring for signs of withdrawal dyskinesias.
References:
Arat-Çelik, H. E., Kök-Kendirlioğlu, B., Çetin, B., & Küçükgöncü, S. (2021). Double-Edged Sword: A Case with Withdrawal-Emergent Dyskinesia. İki Ucu Keskin Bıçak: Nöroleptik Kesilmesiyle Gelişen Diskinezi Olgusu. Turk psikiyatri dergisi = Turkish journal of psychiatry, 32(4), 283–285. https://doi.org/10.5080/u25613
Mejia, N. I., & Jankovic, J. (2010). Tardive dyskinesia and withdrawal emergent syndrome in children. Expert review of neurotherapeutics, 10(6), 893–901. https://doi.org/10.1586/ern.10.58
Pugin, D., Bally, J., Horvath, J., Pollak, P., Gasche, Y., & Burkhard, P. R. (2017). Life-threatening neuroleptic withdrawal emergent syndrome resembling status dystonicus. Parkinsonism & related disorders, 35, 96–97. https://doi.org/10.1016/j.parkreldis.2016.11.006

