Transplant Psychiatry
Session: Poster Session
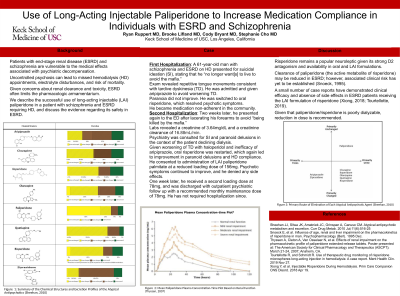
(202) Use of Long-Acting Injectable Paliperidone to Increase Medication Compliance in Individuals with ESRD and Schizophrenia
Trainee Involvement: Yes
- RR
Ryan Ruppert, MD
Resident Physician
University of Southern California
Los Angeles, California, United States 
Cody Bryant, MD
Assistant Program Director, USC/LAC+USC Consultation-Liaison Psychiatry Fellowship
University of Southern California
Los Angeles, California, United States
Brooke Lifland, MD (she/her/hers)
Clinical Assistant Professor of Psychiatry and the Behavioral Sciences
Keck School of Medicine of USC
SOUTH PASADENA, California, United States
Stephanie Cho, MD (she/her/hers)
Director, Consultation-Liaison Psychiatry Services
Keck School of Medicine of the University of Southern California (USC)
Los Angeles, California, United States
Presenting Author(s)
Co-Author(s)
Patients with end-stage renal disease (ESRD) and schizophrenia are particularly vulnerable to secondary medical complication with psychiatric decompensation. Uncontrolled psychosis can contribute to missed hemodialysis (HD) appointments, resulting in electrolyte disturbances and increased risk of mortality. Concerns about renal clearance and toxicity in ESRD often limit the pharmacologic armamentarium. We describe successful use of long-acting injectable (LAI) paliperidone in a patient with schizophrenia and ESRD requiring HD and discuss the available evidence supporting its safety in ESRD. A 61-year-old man with schizophrenia and ESRD was admitted for HD. Psychiatry was consulted for suicidal ideation and paranoid delusions in context of missed dialysis. On psychiatric evaluation, he reported after presenting with suicidal ideation and intent to cut himself due to paranoid delusions, stating he “no longer want[ed] to live to avoid the mafia.” He was given aripiprazole to avoid worsening tardive dyskinesia (TD) which was observed on exam, however paranoia did not improve. Psychotic symptoms rapidly resolved after switching to risperidone, and he was discharged on oral risperidone 2mg twice daily. Two weeks later, he was readmitted for HD and psychiatric evaluation after presenting with self-inflicted forearm lacerations with creatinine of 3.64mg/dL and creatinine clearance of 16.88mL/min. He had not adhered to oral risperidone and had cut himself to “avoid being killed by the mafia.” He declined HD, but did not provide a clear explanation and appeared guarded. Past treatment with haloperidol had worsened TD, and aripiprazole was ineffective. Oral risperidone was restarted and again led to improvement in paranoid delusions and acceptance of HD. After extensive discussion on risk, benefits, and alternatives, the patient consented to administration of LAI paliperidone palmitate at reduced loading dose of 156mg to support psychotropic adherence. Psychotic symptoms continued to improve and he denied any side effects. A second dose of 78mg, administered one week later, was well tolerated. He was discharged with outpatient psychiatric follow up and monthly maintenance dose of 78mg, with no subsequent hospitalizations. Risperidone remains a popular neuroleptic given strong D2 antagonism and availability in oral and LAI formulations. Clearance of paliperidone (the active metabolite of risperidone) may be reduced in ESRD; however, associated clinical risk has yet to be established (Snoeck, 1995). A small number of case reports have demonstrated clinical efficacy and absence of side effects in ESRD patients receiving LAI formulations of risperidone (Xiong, 2018; Tourtellotte, 2019). Dose reduction is recommended as paliperidone/risperidone is poorly dialyzable. Though further study is needed, limited case evidence supports LAI paliperidone as a viable treatment option in selected patients with ESRD. Citations: 1. Snoeck E, et al. Influence of age, renal and liver impairment on the pharmacokinetics of risperidone in man. Psychopharmacology (Berl). 1995;122(3):223-9. 2. Xiong Y, et al. Injectable Risperidone During Hemodialysis. Prim Care Companion CNS Disord. 2018;20(2):17l02212. 3. Tourtellotte R, Schmidt R. Use of therapeutic drug monitoring of risperidone microspheres long-acting injection in hemodialysis: A case report. Ment Health Clin. 2019;9(6):404-407.
Objective:
Case:
Discussion:
Conclusion:

