Neurocognitive Disorders, Delirium, and Neuropsychiatry
Session: Poster Session
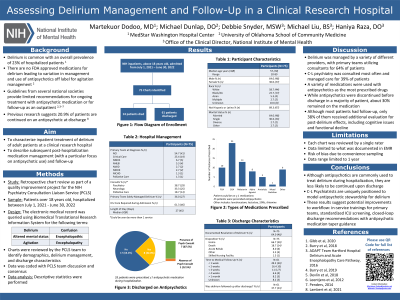
(096) Where Next? Assessing Delirium Management and Follow-up in a Clinical Research Hospital
Trainee Involvement: Yes

Martekuor Dodoo, MD (she/her/hers)
Psychiatrist
MedStar Washington Hospital Center
Washington, District of Columbia, United States- MD
Michael Dunlap, DO
Consultation Liaison Psychiatry Fellow
National Institute of Mental Health
Washington, District of Columbia, United States .jpg)
Deborah Snyder, MSW, LCSW-C, ACC
Faculty, NIH/NIMHPsychiatry Consultation Liaison Service
National Institute of Mental Health
Bethesda, Maryland, United States- ML
Michael R. Liu, B.S.
Research Assistant
National Institute of Mental Health
Rockville, Maryland, United States 
Haniya Raza, DO
Chief, Psychiatry Consultation Liaison Service
National Institute of Mental Health
Bethesda, Maryland, United States
Presenting Author(s)
Co-Author(s)
Delirium is common in hospitalized patients with a prevalence of 20.7% in adult non-intensive care inpatients (Ryan et al., 2013). Management is varied with different care teams, treatment settings, and therapies including antipsychotic medications. However, it is not clear how long the patient should remain on an antipsychotic, particularly after discharge. Guidelines offer limited direction for ongoing treatment with antipsychotic medication or recommendations for follow-up as an outpatient (Burry et al., 2018, 2019; Penders, 2014). This project aims to characterize inpatient treatment, post-hospitalization medication management, and follow-up of adult patients with delirium at a clinical research hospital. This descriptive analysis is part of a quality improvement project within the Psychiatry Consultation Liaison Service (PCLS) at the National Institutes of Health Clinical Center and involves a retrospective chart review of hospitalized patients during a 12-month period (July 1, 2021- June 30, 2022). The electronic medical record was queried for charts within the date range with the terms “delirium,” “altered mental status,” “altered mental,” “encephalopathy” “encephalopathic,” “agitation,” and “confusion” and reviewed by board certified psychiatrists and a licensed clinical social worker from the PCLS to identify subjects with episodes of delirium during hospitalization. Data gathering includes primary diagnoses, primary service, and the presence of psychiatric, neurology, or critical care consultation. The types of delirium treatment, including pharmacologic and non-pharmacologic, are being recorded. Data collection of discharge characteristics includes the number of patients discharged on antipsychotic medications and the type and time to follow-up. Data collection is in progress. Results will include demographic data, patient diagnoses, inpatient management of delirium, and discharge characteristics. Rates of patients discharged on antipsychotic medications and frequency of medical follow-up of delirium post-discharge will be presented. Discussion will be determined following completion of data analysis. Antipsychotic medications are typically used to manage delirium to improve patient safety and reduce undue psychological distress. However, providers should consider the risks of adverse effects with continued use of these medications in patients with resolution of delirium symptoms. Thus, it is important to have a clear process in place for assessment of delirium symptoms and discontinuation of antipsychotics when appropriate to avoid unnecessary use following hospitalization. Burry, L., Hutton, B., Williamson, D. R., Mehta, S., Adhikari, N. K., Cheng, W., Ely, E. W., Egerod, I., Fergusson, D. A., & Rose, L. (2019). Pharmacological interventions for the treatment of delirium in critically ill adults. Cochrane Database of Systematic Reviews, 9. https://doi.org/10.1002/14651858.CD011749.pub2 Burry, L., Mehta, S., Perreault, M. M., Luxenberg, J. S., Siddiqi, N., Hutton, B., Fergusson, D. A., Bell, C., & Rose, L. (2018). Antipsychotics for treatment of delirium in hospitalised non‐ICU patients. Cochrane Database of Systematic Reviews, 6. https://doi.org/10.1002/14651858.CD005594.pub3 Penders, T. M. (2014). Delirium Monograph—Update, Spring 2014. https://www.clpsychiatry.org/wp-content/uploads/DeliriumMonographUpdate2014.pdf Ryan, D. J., O’Regan, N. A., Caoimh, R. Ó., Clare, J., O’Connor, M., Leonard, M., McFarland, J., Tighe, S., O’Sullivan, K., Trzepacz, P. T., Meagher, D., & Timmons, S. (2013). Delirium in an adult acute hospital population: Predictors, prevalence and detection. BMJ Open, 3(1), e001772. https://doi.org/10.1136/bmjopen-2012-001772
Background:
Methods:
Results:
Discussion:
Conclusions:
References:

