Neurocognitive Disorders, Delirium, and Neuropsychiatry
Session: Poster Session
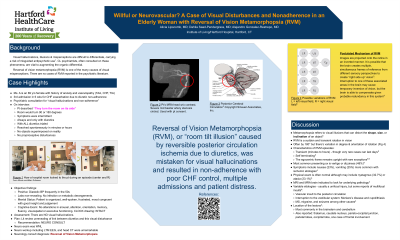
(081) Willful or Neurovascular? A Case of Visual Disturbances and Nonadherence in an Elderly Woman with Reversal of Vision Metamorphopsia
Trainee Involvement: Yes

Alicia Lipscomb, MD
Resident Physician
Hartford Hospital/Institute of Living
Hartford, Connecticut, United States- AG
Alejandro Gonzalez-Restrepo, MD
Staff Psychiatrist
Institute of Living
Hartford, Connecticut, United States 
Dahlia Saad Pendergrass, MD, FACLP
CL Fellowship Director
The Institute of Living/HHC
West Hartford, Connecticut, United States
Presenting Author(s)
Co-Author(s)
Background Elderly patients with cardiac illnesses often require hospitalization. Barriers to timely and accurate diagnosis in this population abound. Caregiver barriers in patients experiencing sensory phenomena include premature closure secondary to misattribution to psychiatric illness. Hallucinations are a common reason for psychiatric consultation, as is perceived patient non-adherence. Disruption of the posterior cerebral circulation can lead to a rare visual phenomenon known as reversal of vision metamorphopsia (RVM) (Yap, 2022). This condition, often caused by disruption to the CNS vestibular functioning, is usually transient and causes a person’s entire field of vision to tilt or flip by 180 degrees (Yap, 2022). This can be misconstrued as visual hallucinations (VH). There is no psychiatric literature on RVM. There is sparse literature on VH with lisinopril, none with diuretics, and none suggesting a connection between diuretic use and RVM (Doane, 2013). We present an 89-year-old woman refusing diuretics for heart failure because they made “the room turn on its side.” Case Ms. A is an 89 yo F with a history of ascending AA, TIA, and anxiety, thrice admitted in six weeks with decompensated HFrEF secondary to noncompliance with diuretics because they caused the “room to turn on its side.” Psychiatric consultation was requested for visual hallucinations and non-compliance. The patient was ambivalent about taking diuretics because while she knew she would feel better and return home, these perceptual disturbances were distressing. She appeared exasperated. She described no objects superimposed on reality, instead the patient’s entire field of vision would intermittently shift 90 or 180 degrees to the left. This happened only after taking her diuretic. She was aware that what she was seeing could not possibly be true. On psychiatric interview, the patient was attentive, her thoughts were logical and consistently reality-based. Neurologic exam was unremarkable for weakness, masking, or rigidity. The CL team encouraged a neurology consult which yielded the elegant explanation that the patient was experiencing diuretic-induced hypoperfusion in the setting of basilar artery stenosis causing RVM. Discussion The CL team is uniquely situated to assist in clinical problems at an impasse by parsing out ambiguous histories. With one ear to the dynamics of patient and caregiver distress and one ear towards clues to the organic medical and neurologic pathophysiology, CL psychiatrists often end up suggesting further investigations to continue workups which then yield answers. We review the literature on RVM, among other visual phenomena with basilar artery disease, and the rare case reports of VH with lisinopril. Implications RVM and this unusual trigger by diuretics will be an addition to CL colleagues’ cache of neurovascular causes of visual disturbances, often misconstrued as psychiatric in etiology and triggering psychiatric consultation. References Doane, J., & Stults, B. (2013). Visual hallucinations related to angiotensin-converting enzyme inhibitor use: case reports and review. Journal of clinical hypertension (Greenwich, Conn.), 15(4), 230–233. https://doi.org/10.1111/jch.12063 Yap JA. Upside-down vision: a systematic review of the literature. BMJ Neurology Open 2022;4:e000337. doi: 10.1136/bmjno-2022-000337

