Neurocognitive Disorders, Delirium, and Neuropsychiatry
Session: Poster Session
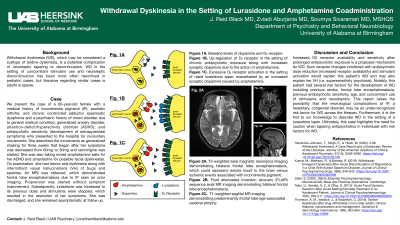
(090) Withdrawal Dyskinesia in the Setting of Lurasidone and Amphetamine Coadministration
Trainee Involvement: Yes

Jonathan R. Black, MD (he/him/his)
Psychiatry Resident
University of Alabama at Birmingham
Birmingham, Alabama, United States
Soumya Sivaraman, MD, MSHQS
Director ECT Services, Assistant Quality Medical Officer
University of Alabama at Birmingham
Hoover, Alabama, United States
Zviadi Aburjania, MD
Psychiatry Resident
University of Alabama at Birmingham
Birmingham, Alabama, United States
Presenting Author(s)
Co-Author(s)
Hendricks-Johnson, T., Singh, E., & Yilanli, M. (2022). 3.98 Withdrawal Dyskinesia: A Case Report and a Systematic Review of the Literature. Journal of the American Academy of Child & Adolescent Psychiatry, 61(10), S259–S260. https://doi.org/10.1016/j.jaac.2022.09.376 Kumar, M., Mattison, R., & Baweja, R. (2018). Withdrawal-Emergent Dyskinesia After Acute Discontinuation of Risperidone in a Child With Autism Spectrum Disorder. Journal of Clinical Psychopharmacology, 38(6), 640–642. https://doi.org/10.1097/JCP.0000000000000958 Tekin, U., Soyata, A. Z., & Oflaz, S. (2015). Acute Focal Dystonic Reaction After Acute Methylphenidate Treatment in an Adolescent Patient. Journal of Clinical Psychopharmacology, 35(2), 209–211. https://doi.org/10.1097/JCP.0000000000000266 Thomson, A. M., Wallace, J., & Kobylecki, C. (2019). Tardive dyskinesia after drug withdrawal in two older adults: Clinical features, complications and management. Geriatrics & Gerontology International, 19(6), 563–564. https://doi.org/10.1111/ggi.13669
Background: Withdrawal dyskinesia (WD), which may be considered a subtype of tardive dyskinesia, is a potential complication of neuroleptic tapering or discontinuation. WD in the setting of concomitant stimulant use and neuroleptic discontinuation has been most often described in pediatric cases, but literature regarding similar cases is adults is sparse.
Case: We present the case of a 60-year-old female with a medical history of incontinentia pigmenti (IP), psoriatic arthritis, and chronic constricted adductor spasmodic dysphonia and a psychiatric history of mood disorder due to general medical condition, generalized anxiety disorder, attention-deficit/hyperactivity disorder (ADHD), and antipsychotic sensitivity (development of extrapyramidal symptoms) who presented to the hospital for involuntary movements. She described the movements as generalized shaking for three weeks that began after her lurasidone was decreased from 60mg to 30mg and lamotrigine was started. She was also taking mixed amphetamine salts for her ADHD and amantadine for possible facial dyskinesias. On examination, she had tremor and dyskinesia along with intermittent visual hallucinations (VH) of bugs and sparkles. An MRI was obtained, which demonstrated frontal lobe encephalomalacia due to IP seen on prior imaging. Propranolol was started without symptom improvement. Subsequently, lurasidone was increased to its previous dose and stimulants were stopped, which resulted in the resolution of her symptoms. She was discharged, and she remained asymptomatic at follow up.
Discussion: Increased D2 receptor availability and sensitivity after prolonged antipsychotic exposure is a proposed mechanism for WD. Such receptor changes combined with antipsychotic dose reduction (increased receptor availability) and stimulant activation would explain this patient’s WD and may also explain her VH (i.e. supersensitivity psychosis). Notably, this patient had several risk factors for the development of WD including previous stroke, frontal lobe encephalomalacia, previous antipsychotic sensitivity, age, and concomitant use of stimulants and neuroleptics. This report raises the possibility that the neurological complications of IP, a hereditary, congenital disorder, may be an under-recognized risk factor for WD across the lifespan. Furthermore, it is the first to our knowledge to describe WD in the setting of a lurasidone taper.
Conclusions: This case describes a unique case of WD and highlights the need for caution when tapering antipsychotics in individuals with risk factors for WD.
References:

