Psycho-Oncology and Palliative Care
Session: Poster Session
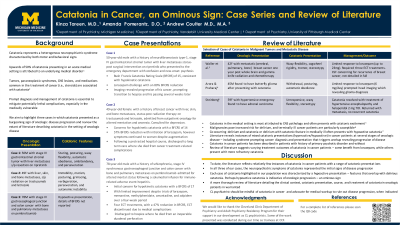
(124) Catatonia in Cancer, an Ominous Sign: Case Series and Review of Literature
Trainee Involvement: Yes

Kinza Tareen, MD
Clinical Assistant Profesor
University of Michigan
Ann Arbor, Michigan, United States
Amanda Pomerantz, DO
Consultation-Liaison Psychiatry Fellow
Vanderbilt University Medical Center
Nashville, Tennessee, United States- AC
Andrew Coulter, MD, MA
Associate Staff
Cleveland Clinic Foundation
Cleveland, Ohio, United States
Presenting Author(s)
Co-Author(s)
Background
Catatonia represents a complex neuropsychiatric syndrome resulting from varied etiologies, both psychiatric and organic. Prompt diagnosis and management is essential to mitigate potentially lethal complications, especially in the medically vulnerable. We highlight three cases in which catatonia presented as a burgeoning sign of oncologic disease progression.
Case Presentations
Case 1
50-year-old male with a history of neurofibromatosis type-1, stage IV gastrointestinal stromal tumor (GIST) with liver metastases status-post surgical intervention on ripretinib who presented to the emergency department with confusion and new-onset psychosis. Psychiatric consultation revealed a Bush Francis Catatonia Rating Scale (BFCRS) of 15, consistent with hypokinetic catatonia. Patient responded to a lorazepam challenge with an 80% reduction in BFCRS. Imaging revealed progression of his cancer, prompting transition to hospice and his passing several weeks later.
Case 2
49-year-old female with a history of breast cancer with liver, skin, and bone metastases, status-post radiation therapy on trastuzumab and letrozole, admitted from outpatient oncology for altered mentation and anorexia. Psychiatry was consulted for depression. Initial psychiatric assessment raised concern for hypokinetic catatonia with a BFCRS of 14. There was an initial 57% reduction of BFCRS following initiation of lorazepam, however symptoms continued to worsen despite augmentation. Following a protracted hospital course, she discharged to long term care where she died from cancer treatment-related complications.
Case 3
78-year-old male with a history of schizophrenia, stage IV synchronous gastroesophageal junction and colon cancer with bone and pulmonary metastases on pembrolizumab admitted for altered mental status following a solumedrol infusion for immune-related adverse event hepatitis. Initial psychiatric assessment raised concern for hypokinetic catatonia with a BFCRS of 17, with limited improvement despite trials of lorazepam, memantine, methylphenidate, amantadine, and zolpidem over a four-week period. Four ECT treatments were completed with a 47% reduction in BFCRS, however ECT was discontinued due to medical complications. The patient was discharged to hospice where he died from an inoperable duodenal perforation.
Discussion
To date, the literature reflects relatively few instances of catatonia in cancer patients. In all three of our cases, the neuropsychiatric symptoms of catatonia represented the initial signs of disease progression. Therefore, we suspect catatonia in this population is an ominous sign that consultation-liaison psychiatrists should be aware of when caring for this vulnerable population. We will review the literature to describe characteristics of catatonia in cancer, treatment response, and the implications on prognosis.
References
1) Tandon R, Walden M, Falcon S. Catatonia as a manifestation of paraneoplastic encephalopathy. J Clin Psychiatry. 1988 Mar;49(3):121-2.
2) Vanstechelman S, Vantilborgh A, Lemmens G. Dexamethasone-induced catatonia in a patient with multiple myeloma. Acta Clin Belg. 2016 Dec;71(6):438-440.

