Catatonia
Session: Poster Session
(010) Catatonia in the Setting of Suspected COVID-19 Associated Autoimmune Rhombencephalitis in a Patient With No Known Psychiatric History
Trainee Involvement: Yes

Kathryn Shirley, DO (she/her/hers)
Resident Physician
Christiana Care
Newark, Delaware, United States- AS
Avni Shah, n/a
Student
Lake Erie College of Osteopathic Medicine
Laurel, Maryland, United States 
Myla R. Pereira, n/a
Medical Student
Nova Southeastern University Dr. Kiran C. Patel College of Osteopathic Medicine
Wilmington, Delaware, United States
John Q. Berlin, DO
Attending Psychiatrist
Christiana Care Health Services
Newark, Delaware, United States
Presenting Author(s)
Co-Author(s)
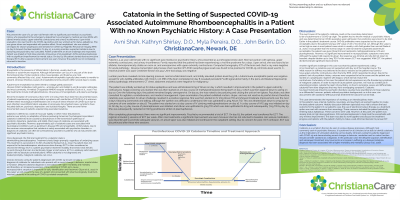
We present the case of a 42-year-old female with no significant past medical/psychiatric history, who presented to the psychiatry consult service with concerns for catatonia in the setting of encephalitis. The patient originally presented to the emergency department with aphasia, upper extremity contractures, urinary incontinence, and mild flu-like symptoms. Reverse transcription polymerase chain reaction (RT-PCR) nasopharyngeal swab was found to be positive for COVID-19. The patient was initially worked up by neurology for status epilepticus and was administered 2mg of Ativan on day 1 of her hospital course which resulted in improvement in the patient’s upper extremity contractures. Keppra 1000mg was started for suspected seizures. On day 15, she was noted by nursing to be posturing and circling the unit on her tiptoes. Upon examination by the psychiatry consult service, the patient was exhibiting mutism, stupor, and was not reactive to painful stimuli, and catatonia was suspected. An ativan challenge resulted in a positive response. The patient was then started on IV 2mg Ativan TID which resulted in mild to moderate improvement over the next 2 days. COVID-19 associated autoimmune rhombencephalitis was suspected by neurology. The patient was started on a 5 day course of IV 1000mg methylprednisolone on day 16, which resulted in minimal improvement. A 3 day course of IVIG 45 G/day was initiated on day 21 which resulted in minimal improvement. On day 24, 5 sessions of plasmapheresis were scheduled. Ativan was uptitrated to 5mg TID, later to 6mg TID and subsequently 7mg TID by day 29 due to restlessness with negativism, verbigeration, impulsivity, Gegenhalten, and preservation. She was started on Vimpat 50mg BID on day 26 for concern for seizures and was taken off Keppra for agitation. She was also continued on 60mg Prednisone daily. Ativan was increased to 8mg TID on day 30 and 9mg TID on day 33 due to minor improvement of catatonia. Repeat MRI obtained on day 34 revealed persistent bilateral mesial temporal and hippocampi signal abnormalities with improvement in pontine signal abnormalities. Plasmapheresis was completed on day 34 which resulted in minimal improvement of encephalopathy, and another 5 day course of IVIG 30 G/day was started. Electroconvulsive therapy was then recommended by psychiatry. Patient began undergoing a taper of ativan and trialed on ECT, three days a week, starting day 63. After 9 treatments, improvement was seen. At this time, there is no further plan to continue ECT as the patient was noted to experience worsening confusion s/p treatment. Thus far, the patient has demonstrated significant improvement; she has not returned to baseline. Unfortunately in this case, Psychiatry was consulted 2 weeks after admission, and it is likely that this patient had developed catatonia early on in her hospital course, resulting in delayed diagnosis and treatment. In this poster, we discuss the challenges and importance of identifying catatonia in the setting of autoimmune encephalitis in a patient with no known psychiatric history. We will also address the difficulty of treating patients who are refractory to standard treatment protocol.

