Quality and Safety
Session: Poster Session
(161) C-L 911! Pilot Implementation of a Behavioral Emergency Response Team Reduces Work-Related Injuries from Patient-to-Staff Violence
Trainee Involvement: Yes
- KH
Kathleen Hanlon, MD
Resident
NYP-Cornell
New York, New York, United States - JP
Jennifer Powell, n/a
Quality and Patient Safety Specialist
New York Presbyterian Hospital
White Plains, New York, United States - SS
Susan Spezzano, MSN RN NEA-BC
Nurse Administrator
New York Presbyterian/Weill Cornell
Shelter Island Hts, New York, United States - RR
Rosanne Raso, RN, DNP, NEA-BC, FAAN, FAONL
Chief Nursing Officer
NewYork-Presbyterian/Weill Cornell
NY, New York, United States - AE
Andrew Edelstein, MD
Assistant Professor
Weill Cornell Medicine
New York, New York, United States 
Jihoon Ha, MD
Psychiatry Attending
New York Presbyterian/Weill Cornell Medical Center
New York, New York, United States- LS
Lisa Sombrotto, MD
Vice Chair, Collaborative and Integrated Care
NewYork-Presbyterian Hospital/Weill Cornell
New York, New York, United States - AD
Anna Dickerman, MD, FAPA, FACLP (she/her/hers)
Chief and Fellowship Program Director, Psychiatry Consultation-Liaison Service
New York-Presbyterian Hospital/Weill Cornell
New York, New York, United States
Presenting Author(s)
Co-Author(s)
Background/Significance: A behavioral emergency response team (BERT) is an interdisciplinary rapid response team for behavioral emergencies, typically on non-behavioral health units where staff members are less prepared to manage them. With increased national focus on reducing workplace harm in healthcare systems, there has been rising interest in utilization of BERTs (Parker, 2020). Though this intervention is of great interest and relevance to consultation-liaison psychiatry, national trends in implementation and literature findings exist mostly in the domain of behavioral health nursing (Loucks, 2010). To our knowledge, there is no current publication describing BERT implementation on a C-L service.
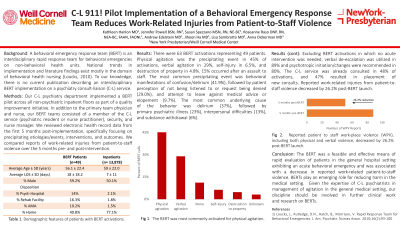
Methods: Our consultation-liaison psychiatry department implemented a BERT pilot across all non-psychiatric inpatient floors as part of a quality improvement initiative. In addition to the primary team physician and nurse, our BERT teams consisted of a member of the C-L service (psychiatric resident or nurse practitioner), security, and nurse manager. We reviewed electronic health record data from the first 6 months post-implementation, specifically focusing on precipitating etiologies/events, interventions, and outcomes. We compared reports of work-related injuries from patient-to-staff violence over the 6 months pre- and post-intervention.
Results: There were 63 BERT activations over the study period. Physical agitation was the precipitating event in 45% of activations, verbal agitation in 29%, self-injury in 6.5%, and destruction of property in 4.8%. 15% occurred after an assault to staff. The most common precipitating event was behavioral manifestations of confusion/delirium (41.9%), followed by patient perception of not being listened to or request being denied (29.0%), and attempt to leave against medical advice or elopement (9.7%). The most common underlying cause of the behavior was delirium (37%), followed by primary psychiatric illness (23%), interpersonal difficulties (13%), and substance withdrawal (6%). Excluding BERT activations in which no acute intervention was needed, verbal de-escalation was utilized in 89% and psychotropic initiation/changes were recommended in 80%. The C-L service was already consulted in 48% of activations, and 47% resulted in placement of new consults. Reported work-related injuries from patient-to-staff violence decreased by 55% post-BERT launch.
Discussion: The BERT was a feasible and effective means of rapid response, assessment, and evaluation of patients in the general hospital setting exhibiting an acute behavioral emergency, most commonly caused by agitated delirium followed by primary psychiatric illnesses. Verbal de-escalation and psychotropic medication were common interventions. The implementation of the BERT was associated with a significant decrease in reported work-related injuries from patient-to-staff violence.
Conclusion: BERTs play an important emerging role for reducing harm in the medical setting. Given the expertise of consultation-liaison psychiatrists in management of agitation in the general medical setting (and particularly delirium), we argue that it is appropriate and necessary for our discipline to be involved in further clinical work and research on BERTs.
References:
Loucks, J., Rutledge, D.N., Hatch, B., Morrison, V. Rapid Response Team for Behavioral Emergencies. J. Am. Psychiatr. Nurses Assoc. 2010;16(2):93-100.
Parker, C.B., Calhoun, A., Wong, A.H., Davidson, L., Dike, C. A Call for Behavioral Emergency Response Teams in Inpatient Hospital Settings. AMA J Ethics. 2020;22(11):E956-964.

