Collaborative and Integrated Care
Session: Poster Session
(054) Clinical and Financial Impact of Integrated "Higher Management" C-L Psychiatric Service
Trainee Involvement: Yes
- PM
Pratheek Mangini, MD
Psychiatry Resident
Temple University Hospital
Philadelphia, Pennsylvania, United States 
Robert E. Simons, MD
Psychiatry Resident
Temple University Hospital
Philadelphia, Pennsylvania, United States- JK
Jessica Kovach, MD
Chair, Department of Psychiatry and Behavioral Sciences
Lewis Katz School of Medicine at Temple University
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Co-Author(s)
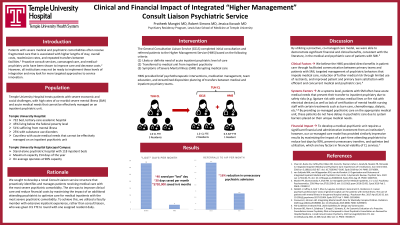
Background: Patients with severe medical and psychiatric co-morbidities often receive fragmented care that is associated with higher lengths of stay, overall costs, readmission rates, and repeated transfers between facilities (Chan, 2018). Proactive consult services, co-managed care, and medical-psychiatry units have been shown to improve care and decrease costs (van Schijndel, 2022). However, not all institutions are ready to implement these levels of integration and may look for more targeted approaches to service innovation. Temple University Hospital treats patients with severe economic and social challenges, with high rates of co-morbid severe mental illness (SMI) and acute medical needs that cannot be effectively managed on an inpatient psychiatric unit. We will describe the clinical and financial impact of a novel Consultation Liaison (CL) service structure targeted towards these patients.
Methods: Prior to intervention, our CL service consisted of one faculty member and 3 psychiatry residents. We sought to maximize the impact of an additional 0.5 FTE attending psychiatrist, with extensive inpatient psychiatry experience, to improve care for medical inpatients with the most severe psychiatric comorbidity. The General Consultation Liaison Service (GCLS) completed initial consultation and referred patients to the Higher Management Service (HMS) based on the following criteria: (1) likely or definite need of acute inpatient psychiatric level of care, (2) transferred to medical unit from inpatient psychiatry, (3) symptoms of SMI disrupting medical care. HMS provided psychotherapeutic interventions, medication management, team education, and streamlined transfer planning between medical and inpatient psychiatry teams.
Results: In the first 6 months of the program, there was a 15 % reduction in the number of patients transferred from TUH to acute inpatient psychiatry. For the patients who were transferred to inpatient psychiatry, the average number of days “lost” waiting for bed availability decreased from an average of 33 to 3 per month. Additional longitudinal data & the economic impact of this project will be presented.
Discussion: Consistent with other innovative CL services, HMS produced positive financial and clinical benefits by targeted identification and co-management of these patients, versus a reactive liaison level of psychiatric support (Muskin, 2016). We will explore the interplay between services provided by HMS, clinical & systems factors, and limitations in generalizing our outcomes.
Conclusions: This study adds to the growing body of literature which exemplifies the benefits of integrated care provided by enhanced consultation liaison psychiatry services in medical hospitals.
References:
Chan AC, Burke CA, Coffey EM, Hilden DR, Coira DL, Warner-Cohen J, Grady M, Muskin PR, Shinozaki G. Integrated Inpatient Medical and Psychiatric Care: Experiences of 5 Institutions. Ann Intern Med. 2018 Jun 5;168(11):815-817. doi: 10.7326/M17-3186. Epub 2018 Apr 24. PMID: 29710091.
van Schijndel MA, van Wijngaarden JDH, van de Klundert JJ. Organization and Outcomes of Integrated Inpatient Medical and Psychiatric Care Units: A Systematic Review. Psychiatr Serv. 2022 Jan 1;73(1):64-76. doi: 10.1176/appi.ps.202000416. Epub 2021 Aug 19. PMID: 34407632.
Muskin PR, Skomorowsky A, Shah RN. Co-managed Care for Medical Inpatients, C-L vs C/L Psychiatry. Psychosomatics. 2016 May-Jun;57(3):258-63. doi: 10.1016/j.psym.2016.02.001. Epub 2016 Feb 2. PMID: 27039157

