Collaborative and Integrated Care
Session: Poster Session
(045) Clinical Challenges Involved in the Psychiatric Care of Patients with Leukodystrophy: A Case Report
Trainee Involvement: Yes

Casey K. Gilman, MD
Resident Physician
Mayo Clinic
Rochester, Minnesota, United States- KU
Kierstin Utter, MD
Psychiatry Resident
Mayo Clinic
Rochester, Minnesota, United States - JE
Jacob K. Ellis, MD
Resident Physician
Mayo Clinic
Rochester, Minnesota, United States .jpg)
Nicholas Allen, MD
CL Program Director
Mayo Clinic
Rochester, Minnesota, United States
Presenting Author(s)
Co-Author(s)
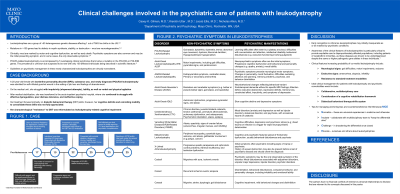
Background/Significance: POLR3-related leukodystrophies are a group of genetic, hypomyelinating diseases that manifest with a wide array of neuropsychiatric symptoms, including mild developmental delay, learning difficulties, attention deficit hyperactivity disorder [ADHD]-like symptoms, and features of conduct/oppositional defiant disorder (Bernard & Vanderver, 2017; Costei et al., 2021). Guidelines on psychiatric management in these newly characterized leukodystrophies are virtually nonexistent. Psychiatrists should be aware of the four clinical signs that would encourage testing for POLR3A: neurologic signs (cognitive deficits, ataxia, dystonia and/or spasticity), abnormal dentition, endocrinologic abnormalities (hypogonadotropic hypogonadism and short stature) and progressive myopia. Earlier recognition of such signs will enable the provision of optimal multidisciplinary care (So et al., 2020). For leukodystrophies, genetic counseling and medical management where possible is critical (Bernard & Vanderver, 2017). Neuropsychological testing can aid the clinical differentiation of personality dysfunction, cognitive impairment or a combination of the two. Finally, the appropriate combinations of cognitive rehabilitation, functional support, pharmacologic management and psychotherapy can be more readily provided. Conclusion/Implications: Leukodystrophies may initially masquerade as or be masked by psychiatric conditions. Increasing awareness of the clinical signs of leukodystrophies may be helpful in earlier recognition of these neuropsychiatric diseases and allow for the needed multidisciplinary care. Bernard G, Vanderver A. POLR3-Related Leukodystrophy. (2017). In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Costei, C., et al. (2021). "Adult Hereditary White Matter Diseases With Psychiatric Presentation: Clinical Pointers and MRI Algorithm to Guide the Diagnostic Process." J Neuropsychiatry Clin Neurosci 33(3): 180-193. So, J., et al. (2020). "High Rates of Genetic Diagnosis in Psychiatric Patients with and without Neurodevelopmental Disorders: Toward Improved Genetic Diagnosis in Psychiatric Populations." Can J Psychiatry 65(12): 865-873.
Case: A 25-year-old female with borderline personality disorder (BPD) and newly diagnosed POLR3A leukodystrophy was admitted for self-inflicted gunshot wound in the setting of job loss and feelings of abandonment. On the medical unit, she struggled with impulsivity and lability, attempting to elope several times, and demonstrating both verbal and physical agitation. After medical stabilization, she was transferred to the acute inpatient psychiatric hospital, where her treatment focused primarily on dialectic behavioral therapy (DBT) skills; however, her cognitive deficits and coinciding inability to consolidate these skills was not fully appreciated. Reflecting on her hospital course, her presumed "resistance" to DBT was contextualized as leukodystrophy-related cognitive impairment.
Discussion: POLR3A-related leukodystrophies often present insidiously and psychiatric symptoms may manifest prior to other neurological signs (Bernard & Vanderver, 2017). Therefore, these diseases typically go undiagnosed for many years and may be managed solely as psychiatric conditions. In this case, our patient had been diagnosed with BPD for many years while experiencing escalating neurologic signs of leukodystrophy, including spasticity, gait instability, and dysarthria. Both conditions worsened, leading to a suicide attempt of highly lethal means. Such cases serve to raise awareness of rare conditions that may be masquerading as psychiatric conditions or masked by them.
References:

