Quality and Safety
Session: Poster Session
(154) Collaboration Between C-L Psychiatrists and Pharmacists to Minimize Medication Reconciliation Errors for Patients Transferred from the Psychiatric C-L Service to the Psychiatric Hospital
Trainee Involvement: Yes

Denise Polaski, MD
Child and Adolescent Psychiatry Fellow
University of Pittsburgh Medical Center Western Behavioral Health
Pittsburgh, Pennsylvania, United States
Priyanka Amin, MD (she/her/hers)
Assistant Professor of Psychiatry
UPMC Western Psychiatric Hospital
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Co-Author(s)
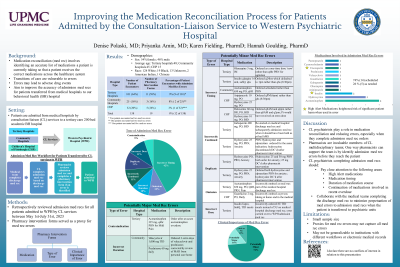
Methods: Data were collected via chart review for patients admitted from medical hospitals via the CL service between May 1st to July 31st, 2021, to three adult psychiatric units with high medical acuity at our institution’s psychiatric hospital. Process measures reviewed include medication reconciliation completion within 24 hours of admission, number of medication reconciliation sources and number of pre-admission medications. The outcome measure of medication reconciliation errors was evaluated based on voluntary pharmacy intervention forms and event reporting records. Results: Forty-one patients were transferred by the CL service during this 3-month period. All medication reconciliations were completed within 24 hours of admission. All had at least one medication reconciliation source of information; 62% used one source and 38% had two or more. 58.5% of patients were on 11+ medications at the time of transfer (range 1-27; average 12.3). No adverse event reports were found, and only one pharmacy intervention form was filed for an incorrect nicotine patch dose. Discussion: To our knowledge, no studies have investigated the effectiveness of collaboration between CL psychiatrists and pharmacists to facilitate complete, timely, and accurate transfer medication reconciliations. We suspect the low rate of adverse event reports and pharmacy intervention forms are due to pharmacists identifying medication reconciliation errors and collaboratively coordinating with the CL service to correct them prior to patient transfers. We expect to have additional data on all medication errors over a 3-month period that were not captured in these data due to informal reporting. We will identify common medication reconciliation errors to be used as targets for physician training to improve the transfer medication reconciliation workflow.
Background: Medication reconciliation is the process of identifying the most accurate list of medications a patient is taking and using this list to provide correct medications for patients anywhere within the healthcare system. Medication reconciliation occurs during times of patient transitions such as transfers from a medical hospital to a psychiatric unit. An estimated 40% of medication errors are due to discrepancies that occur during the medication reconciliation process (Joint Commission, 2016). Our institution’s Consultation-Liaison (CL) psychiatrists collaborate with psychiatric hospital pharmacists to facilitate accurate, timely, and complete medication reconciliation when patients are transferred from medical hospitals to the psychiatric hospital. We aimed to evaluate the effectiveness of this collaboration and to identify potential patient safety targets during these transitions of care.
Conclusion: Collaboration between CL psychiatrists and pharmacists is essential to promote patient safety by minimizing adverse medication events through accurate, timely, and complete medication reconciliations.
References: The Joint Commission. Transitions of Care: Managing Medications, Issue No 26. 2016

